By Andrew Chen, Eunah Kim, MD, Dennis J. Aigner, PhD, Abdelmonem Afifi, PhD, and Joseph Caprioli, MD
Download PDF
Higher health care spending in the United States compared with other countries has not been shown to lead to better outcomes for patients.1 If we are to expand coverage while reducing expenditure, methods to compare cost of resources to quality of care will need to be developed and tested.2
The need for a measure of efficiency. In order to better measure the impact of specific reforms, as well as to compare their effectiveness, the health care system requires a metric of efficiency, representing a function of the ratio of quality to cost per patient. Preliminary measures of efficiency have been proposed for patients with specific diseases, but to our knowledge, none have been suggested to reflect a physician’s practice as a whole.
Calculating an Efficiency Index
In our study, we attempted to develop a metric that estimates the efficiency of ophthalmology practices, with variables representative of practice setting, quality of care, numbers of patients cared for, and total costs.
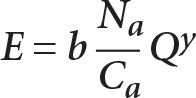
Equation 1—calculating the efficiency index (E). We propose an efficiency index (E), which is defined as a function of adjusted costs (Ca), adjusted number of patients (Na), and quality (Q). Constant b is an empirically determined adjustment factor so that the value of E remains between the limits of 0 and 1. Constant y was set at a value of 2. The higher the value of y, the more the practices with lower quality will be penalized.
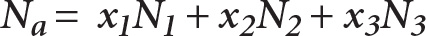
Equation 2—calculating the adjusted number of patients (Na). The adjusted number of patients (Na) was calculated from the number of follow-up patients (N1), new patients (N2), and surgical patients (N3). Adjustments for each type of patient (x1, x2, x3) were empirically derived based on the type of examinations and surgical procedures typically performed on patients in each subspecialty.
Subspecialties in this study included cornea, comprehensive ophthalmology, glaucoma, neuro-ophthalmology, oculoplastics, pediatric ophthalmology, surgical retina, medical retina, and uveitis.
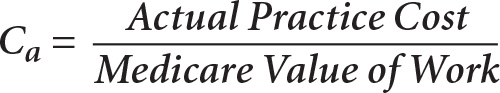
Equation 3—calculating the adjusted cost (Ca). Adjusted cost (Ca) is a variable sensitive to the location of the practice and describes the ratio of the cost of caring for a given group of patients to the Medicare Value of Work. Medicare Value of Work is a function of a) the number of patients, b) Medicare Relative Value Units (RVUs) for each category of patients previously mentioned, and c) geographic practice cost indices. RVUs and geographic practice cost indices are determined by the CMS for each fiscal year. In total, seven inputs from the physician’s practice are required for the calculation of adjusted costs:
- Subspecialty
- Location
- Total number of new patients for a given time period
- Total number of follow-up patients for the same time period
- Total number of surgical patients for the same time period
- Total practice cost for that time period (to care for the reported group of patients)
- The time period under examination
Determining quality (Q). Quality (Q) in this study is a metric of clinical process, as defined by the Donabedian model,3 and was scored by independent auditors masked to patient identities. For each practice, auditors used 20 randomly selected patient charts and used patient-oriented quality questionnaires based on guidelines in the Academy Preferred Practice Patterns. Ten of those charts were used to complete a questionnaire pertaining to a comprehensive eye exam evaluation. The other 10 charts were used to complete a second questionnaire from one of three diagnostic checklists, depending on the subspecialty or stated area of interest: cataract, glaucoma, or age-related macular degeneration.
A separate office-process questionnaire was developed by the Academy Committee for Practice Improvement to address office processes beyond the scope of ophthalmic disease and did not require patient records. This questionnaire focuses mainly on front office performance, workflow, patient communication, incorporation of technology, and safety. Results of the three questionnaires were scored as a percentage, averaged, and then converted to a single value score of Q between 0 and 1 for each practice.
Click here to download the questionnaires used.
The Pilot Study
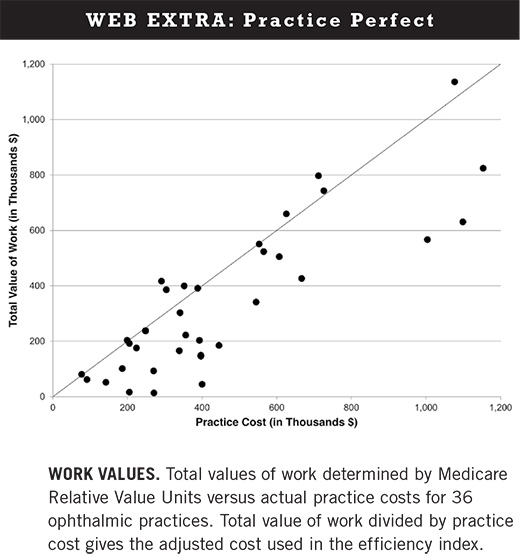
For the pilot study, 36 practices across nine subspecialties in Southern California were included. For these practices, constant b was empirically determined to be 7.0 × 10-5 so that the efficiency index would have a range from 0 to 1. The median quality score was 0.89 with a range from 0.46 to 0.98, and median efficiency was 0.26 with a range from 0.00 to 0.96 (see the Web Extra below for a chart comparing the total value of work to total cost).
The preliminary measure of quality in this efficiency index is based only on the process component of the Donabedian model. It lays a foundation for good outcomes but does not measure outcomes directly. As such, it does not reflect a physician’s performance in its entirety. As real outcome measures become available, these must be added to the calculation of quality.
Furthermore, evidence-based guidelines in ophthalmology do not exist for every disease, and assessing only those patients with conditions that have evidence-based measures may not accurately reflect the scope of a physician’s practice.4 Future work must focus on incorporating appropriately adjusted outcome measures, including patient experience, to more fully evaluate quality.5
In this pilot study, we propose an efficiency index estimated by the cost to run a practice for a measured number of patients as well as the quality of care provided to patients, which was applied to a broad range of ophthalmology subspecialties in Southern California. The efficiency index is easy to calculate and provides a broad overview of performance for a variety of subspecialties as measured by costs and the quality of care delivered. Though all the practices in this pilot study were in Southern California, the efficiency index contains variables, calculated by CMS, that are sensitive to the geographic location of the practice.
To our knowledge, no previous study has integrated location, cost, quality of the care process, and physician performance to evaluate efficiency. As health care reforms are implemented, a metric that incorporates cost will be required to support efforts to increase the value of health care.
___________________________
1 OECD Health Statistics 2013. www.oecd.org/health/healthdata. Accessed May 13, 2014.
2 Mets MB et al. Arch Ophthalmol. 2012;130(9):1195-1198.
3 Donabedian A. JAMA. 1988;260(12):1743-1748.
4 Landon BE et al. JAMA. 2003;290(9):1183-1189.
5 Walter LC et al. JAMA. 2004;291(20):2466-2470.
___________________________
Dr. Caprioli is the David May II Professor of Ophthalmology, Mr. Chen is a senior medical student, and Dr. Kim is a visiting research fellow at the department of ophthalmology, David Geffen School of Medicine, University of California, Los Angeles. Dr. Aigner is emeritus professor of economics and management at the Paul Merage School of Business, University of California, Irvine. Dr. Afifi is emeritus professor of biostatistics at the Jonathan and Karin Fielding School of Public Health, University of California, Los Angeles. Dr. Caprioli chairs—and Dr. Afifi and Mr. Aigner are consultants to—the Academy Committee for Practice Improvement. The authors report no related financial interests.
___________________________
This study was supported in part by the American Academy of Ophthalmology and the Simms/Mann Foundation. The sponsor or funding organizations had no role in the design or conduct of this research.