By Megan A. Rowlands, MPH, and Michael Ehrlich, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Intraorbital foreign bodies (OrbFBs) are a common complication of ocular trauma. Intraocular foreign bodies (IOFBs) are foreign bodies that have penetrated the eye and are lodged within the globe. In contrast, OrbFBs are lodged within the walls of the orbit, which creates a risk of damage to surrounding structures, such as the extraocular muscles and cranial nerves II through VI.
In a study of 62 patients with foreign bodies (FBs) following open-globe injury, the vast majority (85.5%) of FBs were metallic, and 16% of FBs were OrbFBs.1 A retrospective study of metallic OrbFBs by Finkelstein et al.2 showed that 89% of cases were associated with other ocular injuries, including corneal abrasion, iritis, retinal detachment, and commotio retinae. Notably, only 2 OrbFB cases (7.4%) in the study were associated with open-globe injury, and surgical exploration of these did not reveal IOFBs.2
FBs can be difficult to detect and, if missed, may have devastating clinical consequences. The following considerations may help to reduce the potential for harm.
Clinical Assessment
Although the presentation of OrbFBs can vary tremendously, they most commonly occur in males, aged 11 to 30 years.2 When a patient presents with ocular trauma, it is crucial to conduct a thorough investigation, including a complete history and physical examination, along with diagnostic imaging. The clinician should rule out ruptured globe or optic neuropathy, in addition to seeking possible FBs.2,3
Types of FBs. If an OrbFB is detected, it is critical to determine the type of material, which significantly affects management and potential complications.3 Most OrbFBs are metallic, resulting from small particles penetrating the orbit through high-velocity trauma, as with BB pellets.2 Nonmetallic OrbFBs include inorganic materials, such as glass or plastic, or organic materials, such as wood.3
Organic FBs can cause significant inflammation and carry a higher risk of subsequent infection compared with inorganic materials. Inorganic nonmetallic FBs are often inert. However, some metallic FBs, particularly iron, copper, and lead, can cause specific complications such as retinopathy, siderosis, chalcosis, or systemic toxicity.3
The size of the OrbFB also has implications for management. Small fragments are sometimes left in place and observed, depending on the risk posed by surgical exploration.2,3
 |
|
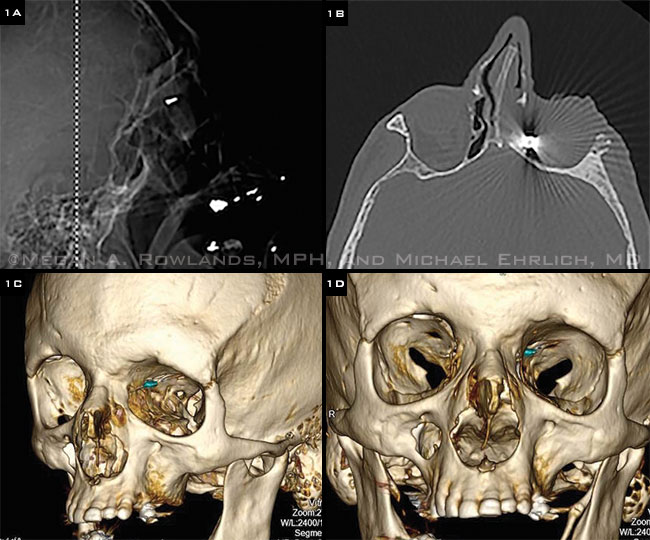
WHAT IS THIS OBJECT? (1A) Intraorbital foreign body detected by CT brain scout image. (1B) Noncontrast CT sinus of same patient, demonstrating significant streak artifact of the OrbFB. This artifact and limited resolution prevented the FB from being characterized. (1C, D) 3-D reconstructions of the noncontrast CT sinus allowed better visualization of the FB. We determined that it was a surgical clip on the ethmoidal artery, which had been placed during a previous sinus surgery.
|
Diagnostic Imaging
Diagnostic imaging is an essential component of the workup to determine the presence, location, material, size, and number of OrbFBs. Imaging options include computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and plain radiography, each of which has particular advantages and limitations.4
CT (Fig. 1A, B). The initial imaging modality of choice for diagnostic evaluation of a suspected OrbFB is a CT scan with thin axial and coronal slices (0.625-1.25 mm).5 It is capable of detecting small FBs (<0.06 mm3) with a sensitivity of over 65%, can be performed relatively quickly, and is generally safe despite radiation exposure. Furthermore, differences in signal intensity make it possible to distinguish between various materials, with wood and plastic displaying low attenuation, compared with graphite, glass, and iron, for example, which appear hyperintense.3,4 It also facilitates diagnosis of possible bony fractures, abscess, and intracranial extension.3
The disadvantages of CT include its cost and occasional obscuration by streak artifacts when imaging iron or glass materials.4
MRI. This modality is generally contraindicated as first-line imaging because the strong magnetic field may dislodge metallic OrbFBs, potentially causing damage to ocular structures or even blindness.3 To avoid this devastating, albeit exceedingly rare, complication, patients are routinely screened for metallic FBs prior to undergoing any MRI,5 usually through use of both questionnaires and radiography.
Once metallic FBs have been ruled out, MRI has advantages over other imaging modalities: It provides better visualization and resolution of soft tissues than CT and does not expose patients to radiation. MRI with T2-weighted and/or contrast and fat suppression protocols is thought to be most sensitive for visualizing OrbFBs and peri-inflammatory reactions.5
The drawbacks of MRI are that it is significantly more expensive and time-consuming than CT,4,5 and fewer facilities are available. While it can detect a variety of materials, such as wood, plastic, graphite, and glass, its ability to differentiate among them is limited. Furthermore, streak artifacts and lower spatial resolution can reduce the quality of the view.4
Other imaging modalities. Plain radiography and ultrasonography (US) are no longer routinely used for evaluation of OrbFBs. Given its low cost and ready availability, plain radiography can be used to screen for and rule out metallic FBs prior to obtaining an MRI. However, it is unable to differentiate metallic FBs from glass or graphite and will miss radiolucent objects, such as plastic and wood. The overall rate of detection of OrbFBs with plain radiography is approximately 40%.3,4
Although US can be more sensitive than plain radiography, the image quality and interpretation vary by user; thus, FBs may be missed completely,3 and their composition and dimensions can not be reliably characterized. Further, there is a relative contraindication against using it on a suspected ruptured globe, due to risk of extruding the vitreous contents.3-5 However, US offers the advantage of allowing the detection of retinal or choroidal detachments and vitreous hemorrhage, which may alter management.
Treatment
Medical treatment. After diagnostic evaluation, all patients with OrbFBs should be treated with antitetanus prophylaxis at presentation.6 If there is a history of recent injury or if signs of orbital infection are present, it is reasonable to give broad-spectrum antibiotics to cover some of the commonly implicated pathogens, such as Bacillus cereus (found in 16%-46% of cases), Staphylococcus (23%-47%), fungal organisms (10%), and polymicrobes (up to 18%).6 In cases of organic FBs, the clinician should consider additional anaerobic coverage.6
Surgical extraction. In deciding whether to extract the FB, the physician must weigh the risk of surgery against the risks of retention, including fistula formation or infection. Surgical removal is usually attempted for all organic OrbFBs because of their higher risk of inflammation and infection.
The removal of inorganic FBs depends on their composition, location, and clinical presentation, and the impairment they cause.2,6,7 A chart review study of 43 patients with metallic OrbFBs that were retained from 6 months to 63 years (median, 2 years) found that they were generally well tolerated.7 Inorganic OrbFBs that are causing orbital complications, such as pain, infection, optic neuropathy, motility disturbance, or hemorrhage, should be removed. However, even in the absence of morbidity, if the FB is located in the anterior orbit, the physician may consider surgery.2,6
Posterior inorganic OrbFBs that are not causing complications are often observed. It is advisable to avoid primary surgical removal in this setting, given the challenge of locating the FB and risks of structural damage.2,7
If the globe is ruptured, it should be repaired and sealed to prevent loss of contents before any orbital exploration for OrbFBs.
Clinical Outcome
The clinical outcome of OrbFBs depends on the severity of the inciting trauma, and the location and material of the FB. Visual loss typically occurs as a result of the initial injury and will be noted at presentation.6
Posterior OrbFBs tend to confer a worse visual prognosis because of their association with traumatic optic neuropathy, while patients with anterior OrbFBs often have at least 20/40 final visual acuity.2 Organic materials elicit greater inflammatory reactions and increase the risk of endophthalmitis and cerebral infection. Surgical extraction itself also carries risks of perioperative or longer-term complications, including infection, optic neuropathy, endophthalmitis, retinal detachment, and proliferative vitreoretinopathy.6 The complications of trauma or surgery may occur insidiously, even months later. Thus, patients should have regular, long-term follow-up.
___________________________
1 Napora KJ et al. Klin Oczna. 2009;111(10-12):307-312.
2 Finkelstein M et al. Ophthalmology. 1997;104(1):96-103.
3 Pinto A et al. Semin Ultrasound CT MR. 2012;33(5):392-395.
4 Lagalla R et al. Eur Radiol. 2000;10(8):1338-1341.
5 Kubal WS. Radiographics. 2008;28(6):1729-1739.
6 Fulcher TP et al. Ophthalmology. 2002;109(3):494-500.
7 Ho VJ et al. Opthal Plast Reconstr Surg. 2004;20(3):232-236.
___________________________
Ms. Rowlands is a medical student, and Dr. Ehrlich is assistant professor of ophthalmology and Director of Oculoplastic and Orbital Surgery. Both are at Yale School of Medicine in New Haven, Conn. Relevant financial disclosures: None.