By Annie Stuart, Contributing Writer, interviewing Carl D. Regillo, MD, Gaurav K. Shah, MD, and Paul E. Tornambe, MD
Download PDF
Treatment of most macular holes has a high success rate with the standard approach—pars plana vitrectomy, internal limiting membrane (ILM) peel, and gas tamponade. In fact, the recent Manchester Large Macular Hole Study found that standard surgical repair had very high success rates in holes up to 650 μm.1
“However, some macular holes don’t always have the same outcomes as regular garden-variety macular holes,” said Gaurav K. Shah, MD, at The Retina Institute in St. Louis. Outliers include large and chronic macular holes and macular holes in highly myopic patients. Holes that have been previously operated on but have failed can also pose a big challenge.
“With these macular holes, you might need to change your techniques to maximize the success rate, but which techniques are best is not yet clear,” said Carl D. Regillo, MD, at Wills Eye Hospital in Philadelphia. “We don’t have Level 1 evidence to guide us with any of these scenarios.” That means doctors must still rely on anecdotal evidence.
Large and Chronic Holes
Although the traditional definition of a large hole is more than 400 μm, this appears to be evolving, said Dr. Regillo. “I think most would agree, however, that a hole north of 600 microns may not respond as well to standard techniques.”
In addition to size, the morphology of the hole may also matter, said Dr. Shah. “If a hole is larger vertically than horizontally, you probably have a better chance of closing it with the standard techniques. This is one reason it’s important to measure hole size at the apex, not the base, said Paul E. Tornambe, MD, at Retina Consultants San Diego in La Jolla, California.
The standard techniques. For large holes not previously operated on, Dr. Regillo does a vitrectomy and hyaloid peel. “I often use triamcinolone to ensure that I’ve got all the vitreous gel up off the posterior pole,” he said. “I use indocyanine green (ICG) stain for the ILM peel. The larger the hole, the larger ILM peel I do. I will also use C3F8 gas. This approach works for me well over 90% of the time.”
For bigger holes, Dr. Tornambe also uses the longer-acting perfluoropropane (C3F8) tamponade, rather than sulphur hexafluoride (SF6). “The bubble acts like a Band-Aid or bridge for healing tissue to cross,” he said.
Adding an ILM flap. Dr. Shah’s standard approach is similar to that of Dr. Regillo and Dr. Tornambe. However, for holes larger than 600 μm, he adds an ILM flap technique. “To do this, you need to preserve the ILM in a way that allows you to cover the hole.”
For holes up to 650 μm, Dr. Tornambe is satisfied with a conventional procedure, and he never uses an ILM flap. There are no prospective, randomized studies that show ILM flaps have a higher anatomic or visual success rate than a complete broad ILM peel, he said. “There is no proof you can close these holes any better with an ILM flap than with a complete broad ILM peel and make the central scotoma smaller,” he said. “If you don’t get photoreceptors in the center of the hole, you won’t achieve decent central vision.”
Dr. Shah agreed that the presence and function of photoreceptors is key. However, he said, the patient’s foveal function might improve due to eccentric fixation. “Although visual acuity outcomes may be variable,” he said, “repairing the hole may still improve vision by increasing depth perception, allowing both eyes to function better together.”
 |
|
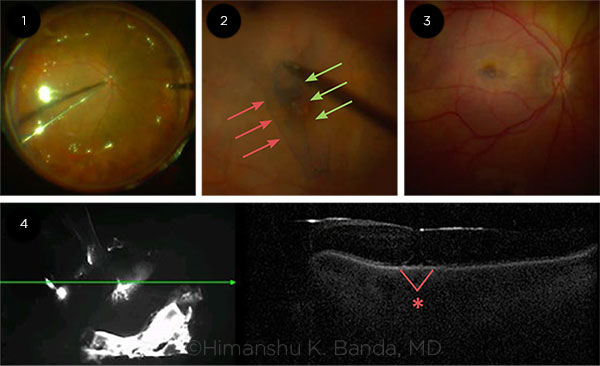
ILM FLAP/FLOWER TECHNIQUE. (1) Passive rather than active extrusion used during air-fluid-exchange to prevent flap decentration. Viscoelastic devices may not be required to fixate the ILM flap/flower if fluid is extruded with minimal turbulence. (2) Engaging ILM peel from both nasal (green) and temporal (red) aspects of the flap. This technique requires initiating a rhexis from both sides, allowing the free edges to “scroll,” covering the hole. (3) After membrane peel, prior to air fluid exchange. (4) First postoperative day exam following repair of full thickness macular hole using ILM flap technique. The hole (asterisk) is closed under gas with trace subretinal fluid.
|
Holes in Highly Myopic Eyes
Hinged flap. For cases of high myopia, particularly with posterior staphyloma, Dr. Regillo adds an ILM hinged-flap technique. After a hyaloid peel and ICG stain, he does a generous ILM peel but leaves the temporal side hinged so he can flap it over the hole. For the gas tamponade, he uses the long-acting C3F8.
Flower flap. Dr. Shah recommends an approach similar to that used for large, chronic holes. “In patients with myopic staphyloma, you need to stain and restain to make sure you’ve removed the cortical vitreous and ILM,” said Dr. Shah. “I then use an ILM flap technique, draping the flap over the hole from both sides—either the nasal or temporal side. I typically use a flower technique where I peel toward the hole and then leave the ILM there. When I do the air-fluid exchange, I can see the ILM go into the hole.”
Other approaches. These cases of myopic staphyloma are challenging for multiple reasons, said Dr. Tornambe. “The staphyloma increases the radius of the retina’s curvature, creating a bigger gap. And if these myopic eyes have lost a lot of choriocapillaris and retinal pigment epithelium cells, the holes will be harder to close because the RPE cells won’t pump out fluid very well.” Although there may be a place for scleral indentation in these patients, said Dr. Tornambe, he does conventional surgery for holes with posterior staphylomas. “If this does not work well, I would try a type of posterior plombage macular push for hole closure.”
Facedown Positioning?
A recent survey by the American Society of Retina Specialists (ASRS) found that 70% of retina surgeons who do macular hole surgery had never tried facedown positioning, said Dr. Tornambe. He never puts patients face down (nor face up) no matter the size of the hole. “As long as the bubble is large enough to be on the trouble, it doesn’t really matter what position the patient is in,” he said.
Dr. Tornambe does strongly advocate using 1% pilocarpine 2-3 times a day for about a week after surgery for eyes that have recently been rendered pseudophakic. This keeps the pupil small and helps prevent iris capture of the lens if the patient happens to lie flat on his or her back while sleeping.
Both Drs. Shah and Regillo do use variations of short-term facedown positioning. “I typically position patients face down for 8 hours a day for 3 days,” said Dr. Shah. “But having a full gas fill—at least a 90% bubble—on Day 1 is most important. At night, patients can sleep on either side, but not flat on their backs.” Dr. Shah typically gets an OCT on Day 1, at which time the hole is often closed. “This gives patients a lot of reassurance.”
Dr. Regillo also recommends 2-3 days of facedown positioning for larger holes or reoperations, but only for as many hours as the patient can tolerate. “If this might boost success rates for larger holes, why not do it?” he asked.
___________________________
1 Koppen C et al. Am J Ophthalmol. 2018;185:43-47.
|
Failed Macular Holes
What if surgery fails to close the hole? A conservative approach may be the best first response, and then you may want to consider other newer techniques.
Remove any remaining tissue. Tangential traction on the ILM may keep a hole from closing, said Dr. Tornambe. “When I find a failed macular hole, I make sure all the ILM is peeled off the hole. Even if there is no ILM around the edges of the hole, I do a much broader peel of the ILM—about a disc diameter radially from the foveal center for 360 degrees, arcade to arcade. If you do less than that, the ILM can still contract and keep the edges of the hole open.”
Add a flap. The most challenging and troublesome failed holes, said Dr. Regillo, are cases where the hyaloid is out, a generous ILM peel has been done, and the hole is still open. “That’s when you’re left with limited options,” he said. “If there is ILM outside the macula, you can peel it away and do a free flap. To do this, you have to use viscoelastic material to help hold the flap in place.”
Other loosening maneuvers. Using Alcon’s Flex Loop, Dr. Regillo has achieved success by loosening up the area of the central macula by making radially directed maneuvers on the surface of the retina toward the hole. “The theory here is that there may be something unidentifiable on the surface that may be holding the hole open,” he said. “Disrupting that tissue may loosen up the edges and make them come together.”
Dr. Tornambe has also made cuts at the edge of the hole to release the traction and tried peeling membrane underneath the retina. However, he cautioned, doing so can peel inner photoreceptors that don’t come back.
Transplantations. “If there is no tissue left for me to peel,” said Dr. Shah, “I do an autologous ILM transplantation.” This involves taking ILM from wherever it exists and placing it inside the hole as a bridge to help glial cells close the hole. “If there isn’t adequate ILM for this procedure, you may try 2 other transplant techniques.”
One is autologous retinal tissue transplantation—a full-thickness retinal graft from the peripheral retina, introduced by Tamer H. Mahmoud, MD, PhD, at Duke Eye Center.2 The other technique, said Dr. Shah, uses amniotic membrane to bridge the gap between the edges of the hole, pioneered by Stanislao Rizzo, MD, with Universitaria Careggi in Florence, Italy.3
Tips for Enhancing the Outcome
Although newer techniques have not been fully evaluated, surgeons can take certain steps to help enhance the chance of success with challenging holes.
Minimize manipulation. “Regardless of the hole size, you want to minimize manipulation of macular tissue and the amount of time in the eye, as well as exposure to the ICG for staining the ILM,” said Dr. Regillo. “All these things can be potentially detrimental.”
Make sure the patient is pseudophakic. Dr. Tornambe recommends that every patient is either pseudophakic or rendered pseudophakic during the vitrectomy surgery. “I do this for a few reasons,” he said. “First, if the patient is older than 50 and has a macular hole, he or she will get a cataract within a year or 2.
“Second, complications are lower. I have never seen the Irvine-Gass syndrome in patients who are pseudophakic or rendered pseudophakic at the time of vitrectomy.” Also, posterior dislocated lenses are less common, he said, because it is easier to do a cataract operation before, rather than after, the vitrectomy operation.
Both Drs. Tornambe and Shah recommend pseudophakia for yet another reason: It helps maximize the amount of vitreous that can be removed, which maximizes the size of the gas bubble. “The bigger the gas fill in chronic or large holes, the greater the chance of success,” said Dr. Shah.
Get an adequate gas fill. “The biggest mistake people make is not having at least an 85% to 90% bubble on Day 1,” said Dr. Shah. “If you make eyes with really big holes pseudophakic, use a 16% C3F8 bubble, and have a 95% or greater fill,” added Dr. Tornambe, “that bubble will be on the trouble in the upright position for about 5 weeks.”
Use sutures. To prevent loss of gas, Dr. Tornambe also sutures the wounds, even if they don’t look like they are leaking at the end of surgery. “If you lose a little bit of gas in a macular hole operation and don’t have a 95% fill on the first day, you will have a problem,” he said.
Practice new techniques on smaller holes. If you want to learn something new, such as an ILM flap, try these techniques first on small or medium holes, rather than on a very large hole, where success may depend upon the extra procedure, said Dr. Shah. If you’re not comfortable trying new techniques, refer to someone who is. “There’s no shame in doing this,” he said.
Manage the fellow eye. Patients with challenging macular holes should be watched carefully for signs of problems in the fellow eye, said Dr. Shah. He advises that OCT be done on the fellow eye each time the patient comes into the office.
___________________________
1 Ch’ng SW et al. Am J Ophthalmol. 2018;195:36-42.
2 Grewal DS, Mahmoud TH. JAMA Ophthalmol. 2016;134(2):229-230.
3 https://retinaroundup.com/2018/07/23/asrs-2018-surgical-symposium/. Accessed Oct 3, 2018.
___________________________
Dr. Regillo is director of the Retina Service at Wills Eye Hospital and professor of ophthalmology at Thomas Jefferson University in Philadelphia. Relevant financial disclosures: Alcon: C.
Dr. Shah is a retina specialist, partner, and codirector of the retina fellowship at The Retina Institute in St. Louis, Mo. Relevant financial disclosures: None.
Dr. Tornambe is president of Retina Consultants San Diego in La Jolla, Calif. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Regillo Aerpio: S; Alcon: C,S; Allergan: C,S; Genentech: C,S; NotalVision: C,S; Novartis: C,S; Regeneron: S; Shire: C.
Dr. Shah Allergan: C,S; Bausch + Lomb: L; Dorc: S; Regeneron: C,L.
Dr. Tornambe Clearside: C,O; Optos: C,L; Optovue: C,L; Poway Retinal Technologies: O,P.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|