Download PDF
Medications, both ocular and systemic, are important iatrogenic causes of acute angle-closure glaucoma (AACG). AACG is an ophthalmic emergency arising from sudden occlusion of the trabecular meshwork by the iris. During an acute attack, patients typically present with marked elevation of intraocular pressure (IOP), corneal edema, ocular pain, headache, blurred vision, and perception of halos around lights. If not treated promptly, prolonged angle closure may result in optic nerve damage and profound vision loss.
One-third of AACG is estimated to be triggered by over-the-counter or prescription medications.1 According to one cross-sectional study, glaucoma patients take, on average, 4.9 oral medications—some of which may increase the risk for AACG—prescribed by 2.1 other physicians.2 Recognition of drugs that have the potential to incite angle closure is paramount in identifying patients at risk for AACG as well as preventing and managing this complication.
Pathophysiology
There are two main mechanisms by which medications can induce AACG: pupillary block and displacement of the lens-iris diaphragm. Understanding these mechanisms is important in determining the appropriate treatment.
Pupillary block. Pupillary block occurs when the pupillary border of the iris comes into contact with the anterior lens and prevents the flow of aqueous humor from the posterior to the anterior chamber. This induces anterior bowing of the iris and subsequent angle closure. Pupillary block most commonly occurs when the pupil is in mid-dilated position, when the iris is most likely to touch the anterior lens surface. Sympathomimetic drugs (e.g., phenylephrine, pseudoephedrine) and parasympatholytic drugs (e.g., atropine, ipratropium) dilate the pupil and thus pose a risk of angle closure through this mechanism.
Lens-iris diaphragm displacement. Anterior effusions of the choroid or ciliary body can move the lens and iris forward as a unit, thus occluding the angle. This phenomenon also occurs with anterior rotation of the ciliary body. Both open and narrow angles can be occluded by this type of pushing mechanism. Medications such as topiramate and escitalopram that expand choroidal or ciliary body volume or increase zonular laxity and lens size can trigger angle closure in this way.
 |
|
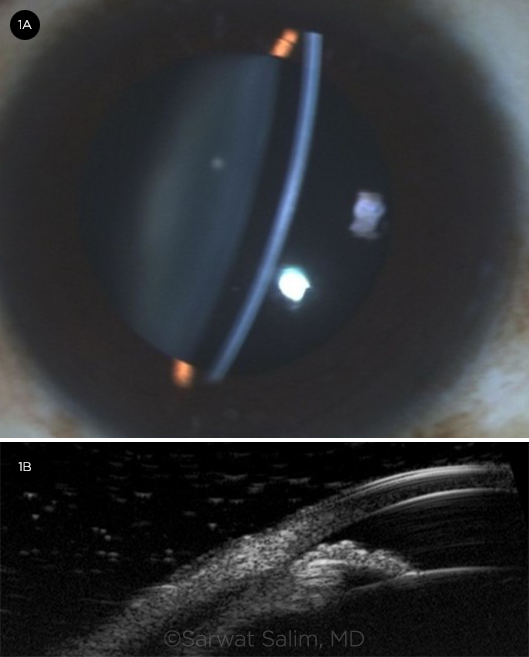
FINDINGS. (1A) Patient has a shallow anterior chamber and (1B) ciliary effusion, which are seen in some cases of medication-induced acute angle closure.
|
Medication Classes
The following medications are among the most common culprits in AACG.
Ophthalmic. Mydriatics are commonly used in ophthalmic practice. Dilating agents with anticholinergic (e.g., tropicamide, atropine) or adrenergic (e.g., phenylephrine) actions pose a hypothetical risk for pupillary block. Among patients who receive diagnostic pupillary dilation, angle closure is estimated to occur in 0.03%.3 Although the risk from a single diagnostic administration of these drugs is low, clinicians should be cautious about the chronic use of mydriatics to treat ocular inflammatory and uveitic diseases.
Pilocarpine, a topical cholinergic, is used as a miotic in the treatment of angle closure due to pupillary block. However, stronger concentrations of pilocarpine have been reported to result in paradoxical induction of angle closure. In addition, pilocarpine can cause anterior displacement of the lens-iris diaphragm through rounding of the lens secondary to contraction of the ciliary muscles.
Psychiatric. Selective serotonin reuptake inhibitors, serotonin-norepinephrine receptor inhibitors, and tricyclic antidepressants are commonly prescribed for the treatment of mood, anxiety, and other psychiatric disorders. Serotonin and serotonergic receptors are present in the eye and have been shown to affect aqueous humor circulation by means of increased aqueous production and mydriasis. Increased noradrenergic and weak anticholinergic effects can contribute to mydriatic pupillary block. Uveal effusions leading to anterior displacement of the lens-iris diaphragm have been reported in patients taking escitalopram.
Benzodiazepines (BZDs) are gamma-aminobutyric acid (GABA) receptor agonists used to treat anxiety, insomnia, and seizure disorders. BZDs also are weakly anticholinergic and can affect pupillary sphincter muscle tone and induce pupillary dilation. Large case-control studies have shown a higher risk of AACG in patients taking BZDs. Use of these drugs in elderly individuals has been associated with angle closure, with a higher risk seen within seven days of starting the medication.4
Neurologic. Topiramate is a sulfa-based antiepileptic medication known to confer a risk for AACG. Patients with topiramate-induced angle closure present with bilateral involvement and large myopic shifts (up to –17 D). Lens edema and supraciliary effusion induced by topiramate contribute to forward movement of the lens-iris diaphragm. Angle closure is most typically seen within two weeks of initiation of topiramate treatment. These effects are believed to be the result of an idiosyncratic drug reaction, which responds to prompt cessation of the drug.5
Respiratory. Over-the-counter (OTC) nasal decongestants and cold remedies often contain phenylephrine or pseudoephedrine. These adrenergic compounds are often paired with antihistamines, which also have anticholinergic effects. The synergistic pharmacology of these compounds can dilate the pupil, inciting pupillary block. Several cases of bilateral angle closure are reported in the literature.
Oseltamivir (Tamiflu) is a therapy for influenza that can induce ciliochoroidal effusions. The mechanism for the effusions is unknown but posited to be an immune-mediated drug reaction.
Nebulized albuterol with ipratropium is a bronchodilator for emergent treatment of acute respiratory conditions. Reports have suggested that these compounds can escape poorly sealed face masks and diffuse through the cornea. The nebulized drugs then exert synergistic beta-adrenergic and anticholinergic effects to incite pupillary block. It is recommended that patients with known risk for AACG wear goggles while being treated with these nebulized compounds.6
Sulfa drugs. Sulfa-based medications include antibiotics (e.g., sulfamethoxazole), diuretics (e.g., acetazolamide, hydrochlorothiazide), insulin secretagogues (e.g., glipizide), and antiepileptics (e.g., topiramate). These drugs are implicated in supraciliary effusions due to an idiosyncratic drug reaction. Topical sulfa-based carbonic anhydrase inhibitors, however, have not been associated with AACG.
Anticoagulants. In rare instances, anticoagulation with heparin can cause spontaneous, massive suprachoroidal hemorrhage leading to forward displacement of the ciliary body and the lens-iris diaphragm. Prognosis is variable, but treatment success has been reported with a sustained course of aqueous suppressants and subsequent pars plana vitrectomy and suprachoroidal drainage of the hemorrhage.7
Neuromuscular blocking agents. Botulinum toxin for cosmetic use or for treatment of blepharospasm can, in rare cases, precipitate angle closure. The toxin is thought to diffuse posteriorly from the injection site to the ciliary ganglion. Its neurotoxic effects at the ganglion inhibit pupillary sphincter function, resulting in dilation and risk for pupillary block.
Diagnostic Approach
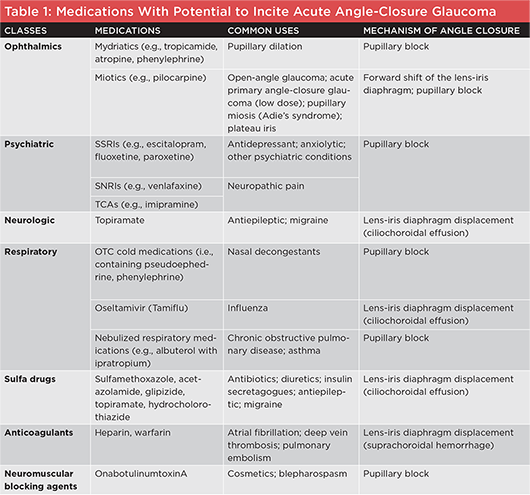
In evaluating AACG, the clinician should conduct a thorough review of a patient’s medications (Table 1, below), paying particular attention to recently started prescription and OTC drugs. Bilateral angle closure presenting with high myopic shifts should raise suspicion for topiramate or sulfa-drug–induced AACG.
A thorough exam, including gonioscopy, should be performed to determine the extent of angle closure. If available, anterior segment imaging with ultrasound biomicroscopy should be obtained to visualize the ciliary body and anterior choroid. This imaging can shed light on the mechanism of angle closure to guide appropriate treatment.
Management
Any medications suspected of inducing angle closure should be discontinued immediately if clinically feasible. Topiramate may require tapering in coordination with the prescribing physician, as abrupt discontinuation can worsen the patient’s underlying epilepsy.
Angle closure caused by a pupillary block mechanism can be treated with miotics, aqueous suppressants, and laser peripheral iridotomy (LPI) to rapidly lower IOP.8 However, LPI will not provide any benefit—and may actually worsen the condition—if the angle closure is caused by pushing mechanisms that displace the lens-iris diaphragm forward. In these cases, prompt discontinuation of the precipitating medication and initiation of topical steroids are effective in reducing the effusion contributing to angle closure.5,9 Cycloplegics may also play a therapeutic role by retracting the ciliary processes and reversing the forward displacement.5
It is essential to inform the prescribing physician of the medication suspected of causing the angle-closure episode. Communication regarding the adverse event will aid in alternative management of the patient’s nonophthalmic condition(s).
|
(Click to enlarge)
|
 |
Identifying and Reducing Risks
Certain groups have higher baseline risk for AACG. These include the elderly; individuals of Asian, Inuit, and Hispanic descent; and females. Biometric features of the eye, such as shorter axial length, larger lens, shallow anterior chambers, and narrow angles, are also predisposing risk factors. Patients with these characteristics should be presumed to be at higher risk of medication-induced angle closure and counseled accordingly.
Gonioscopy is recommended for all at-risk patients but may not be feasible in some clinical settings. Highly hyperopic patients should be prioritized for further exam. For in-patients, the Van Herick technique with the handheld slit lamp can be used to screen for shallow anterior chambers and narrow angles.
High-risk patients should be monitored regularly, with appropriate time allotted for medication review and counseling regarding medications with the potential to incite angle closure. Patients with risk factors for AACG can be offered prophylactic iridotomies prior to initiating treatment with implicated medications, although this has not been formally studied.
__________________________
1 Lachkar Y, Bouassida W. Curr Opin Ophthalmol. 2007;18(2):129-133.
2 Bower T et al. Can J Ophthalmol. 2018;53(3):242-245.
3 Wolfs RC et al. Invest Ophthalmol Vis Sci. 1997;38(12):2683-2687.
4 Park MY et al. J Psychosom Res. 2019;122:1-5.
5 Fraunfelder FW et al. Ophthalmology. 2004;111(1):109-111.
6 Reuser T et al. J R Soc Med. 1992;85(8):499-500.
7 Masri I et al. BMC Ophthalmol. 2018;18(Suppl 1):224.
8 Yang MC, Lin KY. J Curr Glaucoma Pract. 2019;13(3):104-109.
9 Zelefsky JR et al. Am J Ophthalmol. 2006;141(6):1144-1147.
__________________________
Dr. Thieu will be an incoming ophthalmology resident at the Lewis Katz School of Medicine at Temple University, Philadelphia, and Dr. Salim is a professor of ophthalmology, vice chair of clinical and academic affairs, and director of the Glaucoma Service at the New England Eye Center at Tufts University School of Medicine, Boston. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Salim Aerie Pharmaceuticals: C,L; Bausch + Lomb: L.
Dr. Thieu None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|