By Eustace A. Penniecook-Sawyers, MD, and Rohit Adyanthaya, MD
Edited by Steven J. Gedde, MD
Download PDF
Samantha Hendon,* worried about a sudden decrease in the vision of her left eye, consulted her regular ophthalmologist. After examining the 34-year-old teacher, the ophthalmologist ordered laboratory tests for suspected chorioretinitis and sent her to us for a retinal evaluation. Her previous exam performed in that office had noted 20/20 vision in both eyes, with blepharitis being the only abnormal finding.
We Get a Look
Ms. Hendon told us that, during the previous week, the vision in her left eye had become blurry and straight lines had started appearing curvy and wavy. The medical history revealed that she was healthy, although there was a history of diabetes in her immediate family. She reported no ocular redness, pain, floaters, or flashes.
On examination, her best-corrected visual acuity (BCVA) was 20/20 in her right eye and 20/200 in her left, and her refraction results were plano in the right eye and –0.5 D in the left, with no cylinder in either eye. Her intraocular pressure was 14 mmHg in both eyes.
The slit-lamp exam of the anterior segment was normal in both eyes. The fundus exam of the right eye was normal, but the left eye revealed a normal vitreous with a hypopigmented elevated area temporal to the optic nerve. This area measured approximately 1.5 disc areas, involved the fovea, and had radiating striae at its edges (Fig. 1). The remaining retinal exam was unremarkable.
Pinning It Down
At this point, our working differential diagnosis included a pale subretinal mass (such as chorioretinitis, amelanotic melanoma, or choroidal metastasis), an old subretinal hemorrhage, or a choroidal neovascular membrane (CNV).
We reviewed the results of the lab tests Ms. Hendon’s comprehensive ophthalmologist had ordered to determine an etiology for her chorioretinitis. These tests included fluorescent treponemal antibody absorption and rapid plasma reagin tests, a TORCH panel, and a chest x-ray; all results were within normal limits.
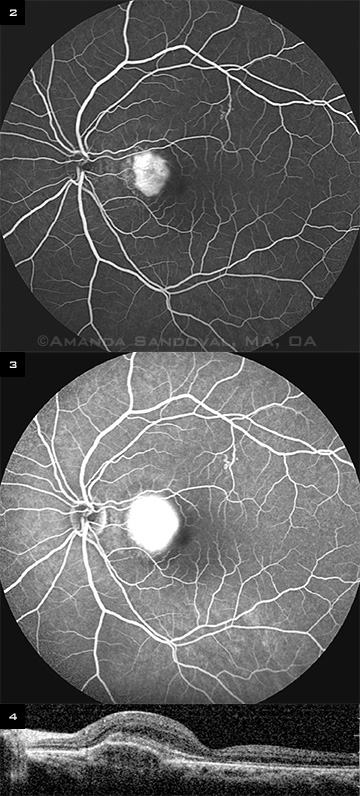
We performed an ultrasound along with a fluorescein angiogram (FA) and optical coherence tomography (OCT) imaging. The FA of Ms. Hendon’s left eye showed an area of hyperfluorescence in the macula in the early phase (Fig. 2), which increased in size and intensity, with blurring of the margins in the late phase (Fig. 3). This was consistent with active leakage and pointed toward the diagnosis of CNV.
Moreover, the OCT of her left eye revealed significant elevation of the pigment epithelium involving the nasal aspect of the fovea with irregular hyperreflectivity under the pigment epithelium. There was no evidence of intra- or subretinal fluid (Fig. 4). Ultrasound did not reveal any retrochoroidal extension.
|
What's Your Diagnosis?
|
 |
|
The fundus photo shows a hypopigmented elevated area measuring approximately 1.5 disc areas and involving the fovea. Radiating striae are evident at the edges of the lesion.
|
Diagnosis and Treatment
Ms. Hendon had no known etiology for CNV, such as high myopia, angioid streaks, or presumed ocular histoplasmosis syndrome. Thus, we diagnosed idiopathic CNV.
After a detailed discussion with our patient, we decided to start her on a series of monthly bevacizumab injections. She was informed that this use of bevacizumab was off label.
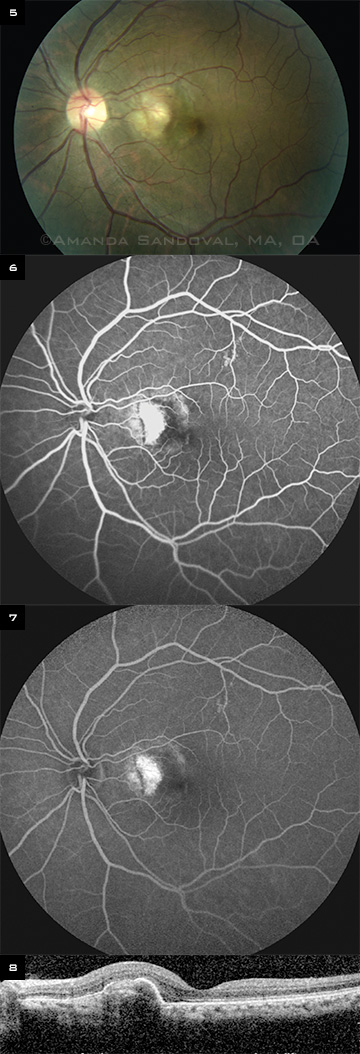
After her third injection, Ms. Hendon’s BCVA improved to 20/40, and she reported that the distortion had improved significantly. There was a substantial decrease in the size of the lesion (Fig. 5). FA revealed a reduction in the size of the membrane with decreased leakage (Figs. 6 and 7), and OCT showed a decrease in the size of the pigment epithelium elevation with improvement in the foveal contour (Fig. 8).
After the fifth injection, Ms. Hendon’s BCVA improved to 20/25 and the lesion stabilized. We then decided to hold off on further injections and to monitor her with biweekly OCTs. She was instructed to use an Amsler grid daily and immediately report back to us if she noticed any new distortion.
The lesion has now been inactive for the last 12 months, and we are monitoring Ms. Hendon every three months.
 |
|
BEFORE TREATMENT. (2) The early phase of FA (at one minute) shows an area of hyperfluorescence in the macula. (3) The late phase (at eight minutes) shows an increase in the size and intensity of the hyperfluorescence with blurring of the margins. (4) OCT reveals elevation of the pigment epithelium involving the nasal aspect of the fovea with irregular hyperreflectivity under the pigment epithelium.
|
Discussion
Etiology. CNV is an uncommon cause of visual loss in patients who are younger than 50 years of age. In one study of 363 patients younger than 50, the etiology of CNV was high myopia in 62 percent; presumed ocular histoplasmosis syndrome in 12 percent; angioid streaks in 5 percent; and miscellaneous hereditary, traumatic, or inflammatory disorders in 4 percent.1 CNV could not be related to any known etiology in 17 percent of the patients and was considered to be idiopathic.
Treatment. A number of treatments have been attempted in patients with idiopathic CNV, including intravitreal and sub-Tenon’s steroid injections, transpupillary thermotherapy, surgical removal, and photodynamic therapy with verteporfin. These have produced varying rates of success.
Recently, intravitreal anti-VEGF treatments have proved effective in patients with CNV of various etiologies, including idiopathic CNV. For instance, Inoue et al.2 reported one-year follow-up of intravitreal bevacizumab in seven patients with idiopathic CNV. In this study, treatment was effective in stabilizing or improving vision.
 |
|
AFTER TREATMENT. (5) After the third injection of bevacizumab, the fundus photo demonstrates a significant decrease in the size of the lesion. (6) In addition, the early phase of FA (at one minute) shows a decrease in the size of hyperfluorescence in the macula. (7) The late phase (at eight minutes) shows decreased leakage. (8) Moreover, a decrease in the size of the pigment epithelium elevation with improvement in the foveal contour is evident on OCT.
|
Conclusion
This case demonstrates the continuing importance of FA in today’s era of OCT imaging as well as the potential benefits of off-label use of selected medications if treatment is provided in a timely and reasonable manner with informed patient consent.
___________________________
* Patient’s name is fictitious.
___________________________
1 Cohen SY et al. Ophthalmology. 1996;103(8):1241-1244.
2 Inoue M et al. Retina. 2010;30(5):733-738.
___________________________
Dr. Penniecook-Sawyers is a vitreoretinal fellow, and Dr. Adyanthaya is an attending retina specialist; both are at Valley Retina Institute in McAllen, Texas. They report no related financial interests.