By Adam C. AüfderHeide, MD, PhD, Mallory Kuchem, OD, MS, John E. Sutphin, MD, and Johnny Tang, MD
Edited by Steven J. Gedde, MD
Download PDF
One morning, Thorfield Stronghammer* had a coughing fit in the shower, but he didn’t think much of it. When he got out of the shower, the 72-year-old retired engineer attempted to insert a contact lens into his right eye. Mr. Stronghammer hadn’t worn the lens for eight months, and he immediately noticed that it felt uncomfortable and threw it away. When he carefully inspected his eye in the mirror, he noticed a white line along the inferior aspect of his iris. He thought this was odd and made an appointment to see us two days later.
We Get a Look
When we saw Mr. Stronghammer, he complained of blurred vision and a “scratched iris” in his right eye. He denied experiencing any recent trauma to that eye but reported the incident with the contact lens.
Mr. Stronghammer’s best-corrected visual acuity (BCVA) was 20/200 in his right eye and 20/25 in his left, and his intraocular pressures (IOPs) were 22 mmHg and 17 mmHg in the right and left eyes, respectively. He had an extensive ophthalmic history that included myopia and Fuchs endothelial dystrophy in both eyes and the following conditions in his right eye: a retinal detachment that had been repaired; cystoid macular edema (CME); and a cataract extraction with zonular dehiscence, vitreous loss, anterior vitrectomy, and posterior capsular opacification.
On initial evaluation, we noted diffuse corneal edema in Mr. Stronghammer’s right eye, along with a dense white infiltrate inferiorly in the anterior chamber that superficially resembled a hypopyon; the anterior chamber was otherwise quiet. Pachymetry showed a central corneal thickness of 704 µm in the right eye and 599 µm in the left. The conjunctiva was white and quiet in both eyes. The posterior exam was unremarkable except for the retinopexy scars associated with his prior retinal detachment repair.
|
What's Your Diagnosis?
|
 |
|
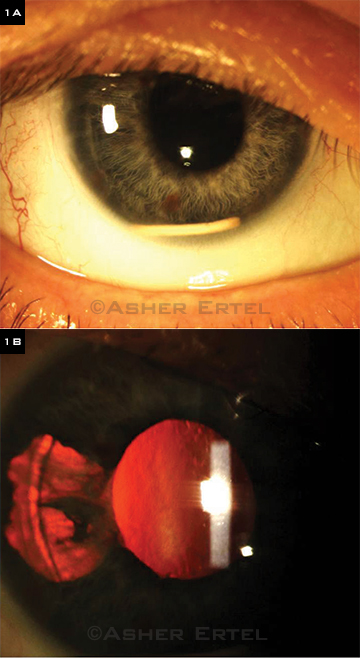
(1A) During the initial evaluation, a large, uniform, solid white mass resting inferiorly in the anterior chamber could be seen in the patient’s right eye. (1B) In addition, a large temporal iris transillumination defect was noted.
|
Differential Diagnosis
Our initial differential for a hypopyon included infectious etiologies, iridocyclitis, systemic drugs, ghost-cell glaucoma, a retained foreign body, and new trauma. We were particularly concerned about the potential presence of endophthalmitis or inflammation, given his recent history of ocular surgeries as well as his misadventure with the contact lens.
On closer inspection, the white material appeared to be a large uniform solid white mass that rested inferiorly in the anterior chamber (Fig. 1A). We also noted a large temporal iris transillumination defect (Fig. 1B).
When we questioned him further, Mr. Stronghammer reported that he had recently seen an outside retina specialist and that, two weeks previously, he had received “some sort of injection for the swelling in the back of the eye.”
Mr. Stronghammer then went on to describe the injection as “something like a rice pellet,” and he recognized the name Ozurdex when he heard the word. During this same visit, our retina specialist confirmed that the mysterious white material in Mr. Stronghammer’s eye was indeed a dexamethasone implant.
Discussion
Ozurdex, the intravitreal dexamethasone implant, is designed for controlled release of medication in the vitreous space.
The biodegradable implant is injected into the vitreous cavity with a 23-gauge delivery device, and it is approved by the U.S. Food and Drug Administration for two indications: 1) CME secondary to branch or central retinal vein occlusion and 2) noninfectious uveitis. The implant’s dimensions are typically 6 mm in length and 0.46 mm in diameter, and it delivers 0.7 mg of dexamethasone.
Migration of the implant into the anterior chamber has been previously described in aphakic patients as well as in patients with iris-claw fixated intraocular lenses (IOLs).
In one study, researchers described three post-lensectomy-vitrectomy aphakia eyes in which migration had occurred because of changes in patient posture.1 Another case report described a 65-year-old woman with a history of multiple retinal detachment surgeries, iris-claw IOL fixation, and persistent CME.2
Corneal decompensation is a risk when the Ozurdex implant moves into the anterior chamber, likely due to contact with the endothelium. This was particularly problematic in our patient, given the history of Fuchs endothelial dystrophy.
Other potential problems caused by migration of the implant to the anterior chamber include loss of effectiveness of the drug delivery system, unpredictability of the implant’s rate of degradation, and risk of damage to adjacent structures. Repositioning of the implant using a 30-gauge needle has been described; however, this was not possible in our patient, because there was no obvious passage back to the vitreous cavity.
To our knowledge, this is the first report of migration of a dexamethasone implant to the anterior chamber in a pseudophakic patient with the IOL situated in the capsular bag. A region of zonular dehiscence that was noted during cataract extraction most likely provided the route by which the implant migrated anteriorly.
Follow-Up
We started Mr. Stronghammer on hypertonic sodium chloride ointment and brimonidine in the right eye. One week later, his BCVA had improved to 20/50, and pachymetry in his right eye was reduced to 661 µm. His IOP was 17 mmHg in his right eye and 14 mmHg in his left.
After discussion with Mr. Strong-hammer, we elected to continue to observe him and to leave the implant alone, as his vision and pachymetry had improved and his pressure was controlled.
We scheduled him for close follow-up to monitor his IOP and corneal status as well as to ensure that the CME does not return.
___________________________
* Patient name is fictitious.
___________________________
1 Bansal R. et al. J Ophthalmic Inflamm Infect. 2012;2(1):1-5.
2 Vela JL et al. Int Ophthalmol. 2012;32(6): 583-584.
___________________________
Dr. AüfderHeide is a resident in ophthalmology, Dr. Kuchem is clinical instructor of ophthalmology, Dr. Sutphin is professor of ophthalmology, and Dr. Tang is associate professor of ophthalmology; all are at the University of Kansas Medical Center in Kansas City. The authors report no related financial interests.
Further Reading
To learn more about the phenomenon of migrating implants, check out the case series by Kurhana RN et al., “Dexamethasone implant anterior chamber migration,” in the January 2014 Ophthalmology. This article was published just as EyeNet was going to press.
|