By Ilyse S. Kornblau, BA, Gerald Campbell, MD, and Brian Wong, MD
Edited by Steven J. Gedde, MD
Download PDF
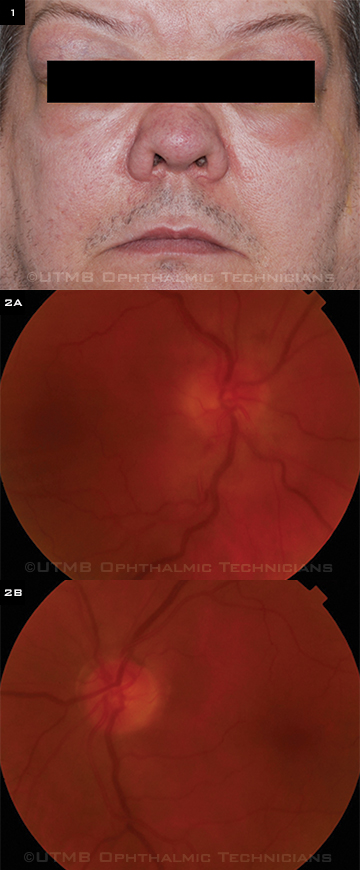
John Haley* was tired of hiding from the camera. Always shy when it came to having his picture taken, the 50-year-old had grown increasingly resistant to being photographed because of facial swelling (Fig. 1). The swelling initially started in the upper outer quadrant of each eyelid. Over a three-year period, it had expanded to the point that it was now causing significant visual impairment. Mr. Haley’s vision was now blurry enough that, even with correction, he had to close his right eye while driving.
We Get a Look
When we saw Mr. Haley, he complained of feeling increasingly “cross-eyed” for the previous two weeks. He also reported eye redness, dryness, and pain (rating 3 or 4 on a scale of 1 to 10), but no irritation or photophobia. In the past, he said, the swelling occasionally diminished in size after he took oral methylprednisolone (Medrol Dosepak) for sinusitis, but it never completely resolved.
Mr. Haley’s history included obesity, hypertension, diabetes, obstructive sleep apnea, and claustrophobia. He had been seen at a nearby institution three years earlier for similar ocular complaints and received a complete workup, including a biopsy of his left lacrimal gland. However, the results were inconclusive—and before definitive treatment could be determined, he lost his medical insurance.
When we examined him, Mr. Haley’s visual acuity was 20/80, improving to 20/60 -1 with pinhole in his right eye, and 20/60 without improvement in his left. His pupils were 6 to 7 mm bilaterally without relative afferent pupillary defect. The visual fields were full to confrontation, and the intraocular pressure (IOP) was 32 mmHg in his right eye and 41 mmHg in his left.
Mr. Haley’s motility was restricted in both eyes in all cardinal gaze directions, with maximum limitation in supraduction (-3). The medial and lateral gaze were equally limited (-2) with almost full motility with infraduction (-1). He had a right esotropia of 8 prism diopters in the primary position.
When we lifted his eyelids, we could see firm, prominent, and erythematous lacrimal glands protruding bilaterally. Exophthalmos measured 32 and 31 mm by Hertel exophthalmometry. In addition, Mr. Haley had firm bilateral enlargement of his parotid and submandibular glands.
On the slit-lamp exam, the conjunctiva had 2+ injection and chemosis bilaterally. The funduscopic exam revealed that the right optic nerve had a blurred disc margin with grade 1 disc edema, inferior splinter hemorrhages, and engorged and tortuous venules, while the left optic disc margin was sharp without edema or atrophy (Figs. 2A-B).
|
What's Your Diagnosis?
|
 |
|
WHAT’S YOUR DIAGNOSIS? (1) The patient had bilateral lacrimal and parotid gland enlargement. (2A) The right fundus photo shows disc edema and engorged tortuous venules; (2B) the left fundus photo shows a normal optic nerve.
|
Differential Diagnosis
The list of disorders that can cause chronic inflammatory orbital masses is lengthy and includes Castleman disease, granulomatosis with polyangiitis, idiopathic orbital inflammation, leukemia, lymphoid hyperplasia or lymphoma, Mikulicz disease, mumps, sarcoidosis, Sjögren syndrome, syphilis, thyroid eye disease, and tuberculosis. Although most of these disorders can be diagnosed with laboratory tests and imaging, a definitive diagnosis is best made with a biopsy.
According to the previous workup from the other institution, Mr. Haley was positive for antinuclear antibodies (ANA) and negative for tuberculin purified protein derivative (PPD) antibodies, and he had a clear chest x-ray. A biopsy taken at that time indicated that he had a sclerosing inflammatory tumor with reactive lymphoid hyperplasia. Flow cytometry did not reveal monoclonality or malignant lymphoma.
Making the Diagnosis
To delineate tumor location and select an appropriate biopsy site, we ordered a CT scan of Mr. Haley’s orbits. However, due to his physical size and symptoms of claustrophobia, neither CT scanning nor magnetic resonance imaging could be completed.
We performed a bilateral anterior orbitotomy with incisional biopsies. On entry into the superolateral orbit, it was evident that firm yellow-white masses were infiltrating the lacrimal glands. Pathologic analysis revealed lymphoid hyperplasia; histology revealed characteristic germinal centers without monoclonality.
Mr. Haley had Mikulicz disease.
Discussion
Mikulicz disease is defined as symmetrical swelling of at least two pairs of lacrimal, parotid, or submandibular glands for more than three months. The disease can be caused by numerous etiologies, from the infectious (syphilis, mumps, tuberculosis) to the neoplastic (lymphoma, leukemia) and the autoimmune (Sjögren, lupus).
Recent research from Japan has shown Mikulicz disease to be related to a group of autoimmune disorders with elevated levels of immunoglobulin G4 (IgG4), which are collectively known as IgG4-related disease (IgG4RD). These disorders include idiopathic orbital inflammation (orbital pseudotumor),1 and some researchers argue that IgG4RD should be renamed IgG4-associated sialadenitis/dacryoadenitis.2
Mikulicz versus Sjögren. Mikulicz disease was discovered in the late 19th century and was later classified as a subset of Sjögren syndrome. However, the two conditions have distinctive epidemiologic and histologic features.3
Although patients with both diseases present with sicca symptoms, those with Sjögren tend to be female, have arthralgias, and have a moderately elevated IgG with positive ANA, anti-SSA, and anti-SSB test results. Biopsies of the affected glands reveal predominantly lymphocytic infiltrate.
In contrast, patients with Mikulicz disease are typically male, have gland swelling and nasal obstruction, and have an elevated IgG with negative ANA, anti-SSA, and anti-SSB results. Biopsies typically show a multitude of lymphocytes and plasma cells with excess IgG4-positive cells and a high IgG4:IgG ratio.
Ruling out Sjögren is key in evaluating patients with multiple glandular masses, as this will affect treatment decisions. For instance, although Mikulicz disease responds to high-dose steroids, Sjögren does not have a good long-term response to steroid therapy.
Back to Our Patient
Our primary concern for Mr. Haley was the possible malignant transformation of his lacrimal, parotid, and submandibular masses, as orbital lymphoid hyperplasia has been reported to progress to non-Hodgkin lymphoma. For instance, in one study, up to one-third of cases progressed to lymphoma over a two- to six-year period; slightly less than half of patients were disease-free at 10 years. Lacrimal gland involvement increased the risk of progression.4
Moreover, orbital lymphoid hyperplasia may be the first sign of systemic lymphoma. As a result, all patients should have a full workup for lymphoma at the time of diagnosis, with regular follow-up by ophthalmologists and oncologists. The inflammatory component may be treated with systemic steroids, and radiation therapy may be necessary.4
At his initial visit, we started Mr. Haley on 60 mg/day of prednisone to treat his severe inflammation and decompress his right optic nerve. Additionally, we prescribed brimonidine (Alphagan) and latanoprost (Xalatan) drops for his elevated IOP.
Two weeks after the anterior orbitotomy, the follow-up exam revealed significant decrease in the size of all of his lesions. At this point, Mr. Haley reported that he was able to consistently wear his glasses and that his vision had markedly improved. In particular, the sensation of being cross-eyed had resolved entirely.
We recommended a slow prednisone taper as the inflammation continues to resolve. In addition, because of the chronic nature of the disease and possible transformation to lymphoma, we referred Mr. Haley to our oncology department for a discussion of radiation therapy.
___________________________
* Patient’s name is fictitious.
___________________________
1 Umehara H et al. Mod Rheumatol. 2012; 22(1):21-30.
2 Geyer JT, Deshpande V. Curr Opin Rheumatol. 2011;23(1):95-101.
3 Takahashi H et al. J Autoimmun. 2012;39(1-2):93-96.
4 Polito E, Leccisotti A. Graefes Arch Clin Ophthalmol. 1996;234(3):150-154.
___________________________
Ms. Kornblau is a fourth-year medical student, Dr. Campbell is professor of pathology and director of anatomic pathology, and Dr. Wong is associate professor of ophthalmology and visual sciences; all are at the University of Texas Medical Branch in Galveston. The authors report no related financial interests.