By Alan T. Sheyman, MD, Ben Z. Cohen, MD, Ebrahim Elahi, MD, Alan H. Friedman, MD, and Nathaniel Wisch, MD
Edited by Steven J. Gedde, MD
Download PDF
Bessie Johnson* was worried. Over a two-month period, she had noticed that the vision in her right eye was becoming progressively dimmer. The 92-year-old woman consulted an ophthalmologist and was referred to us for evaluation of decreased vision and peculiar deposits on her posterior chamber intraocular lens (PCIOL) implant.
We Get a Look
By the time Mrs. Johnson was referred to us, she had undergone a workup that included a chest x-ray; complete blood count and basic metabolic panels; and testing for angiotensin-converting enzyme, Lyme antibody, and rapid plasma reagin levels. All results were within normal limits.
Mrs. Johnson’s ophthalmic history included uncomplicated cataract surgery in her right eye with placement of the PCIOL; this had taken place 20 years previously.
More recently, she had experienced an episode of acute anterior uveitis in her left eye; this occurred about a year before we saw her and had resolved with topical corticosteroids. Her reported medical history included well-controlled hypertension.
On examination, Mrs. Johnson’s best-corrected visual acuity (BCVA) was 20/100 in her right eye and 20/30 in her left. No relative afferent pupillary defect was present. Applanation pressures were 19 mmHg in both eyes.
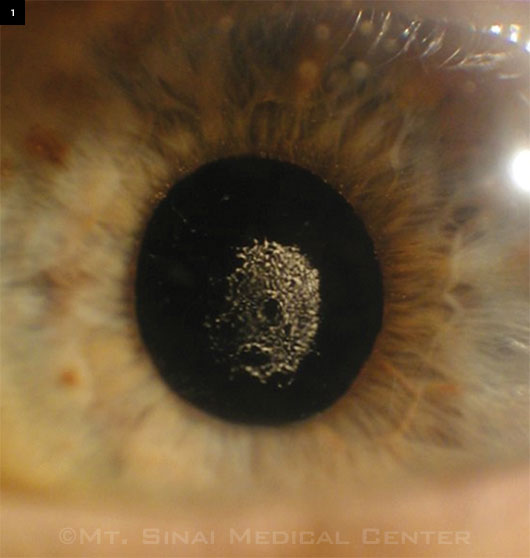
The anterior exam was unremarkable in the left eye. However, in the right eye, comma-shaped keratic precipitates were noted on the endothelium, with evidence of agglutinates just above the pupillary border in the anterior chamber, but without frank cells or flare. There were two small white nodules on the anterior surface of the right iris superiorly. The left iris was unremarkable. Gonioscopy was significant for irregular white deposits in the inferior angle of the right eye. Notably, there were numerous central deposits on the anterior implant surface and on the posterior lens capsule (Fig. 1). The lens was not displaced, and there were no deposits in the bag peripherally. A few similar white deposits were noted in the anterior vitreous. The remainder of the vitreous was unremarkable. There were mild retinal pigment epithelium changes in the maculae of both eyes.
|
What's Your Diagnosis?
|
 |
|
The anterior segment and lens capsule at presentation.
|
Pinning It Down
The differential diagnosis of iris nodules includes iris freckles, juvenile xanthogranuloma, leiomyoma, leukemia, and melanoma. Malignancies can also result in distorted pupils, anterior chamber angle deposition, and iris neovascularization.
The differential diagnosis of deposits on the surface of an IOL includes pseudoexfolation material, uveitis, endophthalmitis, retained lens material, and blood, as in UGH (uveitisglaucoma-hyphema) syndrome.
Because of the peculiar nature of the iris nodules, the aggregates in the inferior anterior chamber angle, and the deposits on the anterior lens surface and the posterior capsule, we homed in on a possible diagnosis of metastatic carcinoma.
Crucial Details Emerge
Upon further questioning, Mrs. Johnson admitted that she had undergone a lumpectomy for breast cancer about a year previously, and she noted that she had refused any further treatment at that time.
A review of the pathology database at our institution revealed that Mrs. Johnson had been diagnosed with infiltrating ductal and lobular carcinoma. The stain for estrogen receptor protein was positive, while the stains for progesterone receptor protein and HER2/neu oncoprotein were negative. Fluorescence in situ hybridization for HER2/neu also was negative. A metastatic workup performed at that time had not revealed any metastases.
 |
|
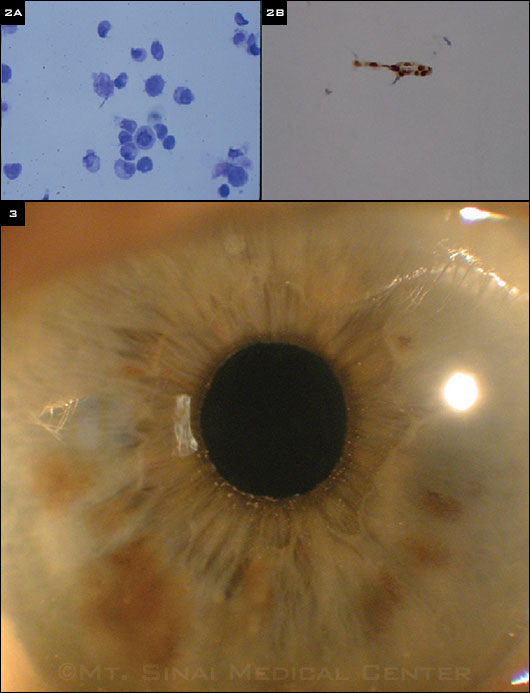
Histology and Resolution. The aspirate from the IOL surface demonstrated (2A) pleomorphic cells with mitotic figures and (2B) estrogen receptor protein–positive staining. (3) The anterior segment and lens capsule after pars plana vitrectomy and treatment with anastrozole.
|
Treatment
Mrs. Johnson was offered a pars plana vitrectomy, to which she agreed. The deposits on the anterior surface of the PCIOL were aspirated, and the histopathologic examination of this aspirate revealed pleomorphic cells with mitotic figures (Fig. 2A). The material was stained for estrogen receptor and was found to be positive (Fig. 2B).
After the pars plana vitrectomy, our oncology colleagues recommended that Mrs. Johnson receive the breast cancer drug anastrozole. She agreed to this therapy and was treated with 1 mg per day. The resultant BCVA in her right eye is now 20/30, and the metastatic deposits and iris nodules have resolved (Fig. 3).
Discussion
Systemic malignancies are well known to metastasize to various structures of the eye. A number of findings—including iris nodules, pseudo-hypopyon, anterior uveitis, and hyphema—have been reported in the literature. Breast cancer is the most common tumor to metastasize to the eye, followed by lung cancer. Other sites of origin include gastrointestinal, prostate, renal, and other tumors, although these account for a smaller percentage of ocular metastases.
Solomon et al. reported native lens capsular opacities from metastatic cutaneous melanoma.1 Pandit et al. reported a case of a patient with crystalline deposits on a PCIOL that led to a diagnosis of a parathyroid adenoma.2 To date, we have not found any other reports of malignancies that metastasized to the anterior chamber with clusters of malignant cells adherent to an IOL.
Our case highlights the importance of using clinical findings and suspicions to elicit additional details of a patient’s medical history that may clarify the ocular and visual findings. Moreover, it serves as a potent reminder that explaining the underlying causes of visual symptoms may prompt patients to reconsider opportunities for systemic treatment of their medical conditions.
In this instance, when Mrs. Johnson was initially diagnosed with breast cancer, she refused chemotherapy. However, when she understood that the malignancy had caused a substantial decrease in vision, she agreed to treatment, which ultimately improved both her medical condition and her vision.
___________________________
* Patient’s name is fictitious.
___________________________
1 Solomon JD et al. Graefes Arch Clin Exp Ophthalmol. 2011;249(1):127-131.
2 Pandit RJ et al. Lancet. 2010;375(9714):610.
___________________________
Dr. Sheyman is chief ophthalmology resident, Dr. Cohen is assistant clinical professor of ophthalmology, Dr. Elahi is assistant clinical professor of ophthalmology, and Dr. Friedman is clinical professor of ophthalmology and pathology; all are at Mount Sinai Medical Center in New York. The authors report no related financial interests.
Editor’s note: One co-author, Nathaniel Wisch, MD, was omitted from the print version of this article. Dr. Wisch is faculty at the Icahn School of Medicine at Mount Sinai in the Department of Oncology. Financial disclosure: None.