Download PDF
Optic nerve hypoplasia (ONH) is an important cause of congenital visual impairment in children and infants. It is a unilateral or bilateral malformation of the optic nerve with a wide spectrum of severity. It has numerous clinical correlates, including neurologic and endocrine pathologies, making timely clinical diagnosis and further investigation crucial.
Prevalence and Epidemiology
Along with cortical vision impairment and retinopathy of prematurity, ONH is thought to be one of the most common causes of impaired vision in children under the age of 3 years. It is estimated that 15% to 25% of infants with significant visual impairment have ONH.1,2
Reported incidence ranges between 2.4/100,000 residents (<19 years of age) annually in Olmsted County, Minnesota, to 17.3/100,000 residents (<18 years of age) annually in Stockholm, Sweden.3,4 There is no clear evidence of variation across geographic regions, but a study based in the United Kingdom found higher standardized incidence ratios in inner-city districts of high population density.4
Risk factors. Although the etiology is unclear in the majority of cases, there are known associations with fetal alcohol syndrome, maternal diabetes, and young maternal age. Other risk factors include maternal primiparity, alcohol or drug use by the mother, intrauterine growth restriction, prematurity, and low birth weight.
Pathophysiology
Impairment of optic nerve development and failure for a normal number of axons to form during the first or second trimester of pregnancy lead to ONH. The retinal nerve fiber layer (RNFL) and ganglion cell layer may be thinned, while the outer retinal layers and vasculature tend to be normal.
Although ONH is generally considered to be a sporadic disease with a multifactorial etiology, a heritable component may play a role in a minority of cases. For example, an association has been postulated between ONH and a mutation in the HESX1 transcription regulation gene, given that both may be seen in patients with septo-optic dysplasia who also manifest pituitary dysfunction. Other proposed gene associations include OTX2 and PROKR2.5
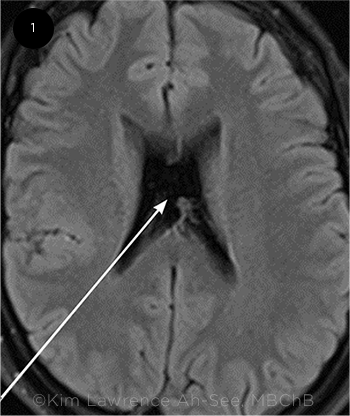
Neurodevelopmental or neuroendocrine disorders may also be associated with ONH, especially in bilateral or severe cases.4 In these patients, ONH can be considered part of a broader multisystem syndrome, which was formerly thought to be synonymous with septo-optic dysplasia (or de Morsier syndrome); however, these terms are now controversial and outdated. Borchert et al. proposed instead “the syndrome of optic nerve hypoplasia.”6 Although there may be an association with congenital absence of the septum pellucidum (Fig. 1), the prevalence of this abnormality in the healthy population is not clear, and it does not necessarily predict severity of disease in ONH.
Nevertheless, congenital midline brain disorders such as hypoplasia or agenesis of the corpus callosum and pituitary malformations are commonly associated with ONH, as are hydrocephalus and arachnoid cysts.5 Hypothalamic dysfunction is the most commonly seen clinical comorbidity.
 |
|
BRAIN ABNORMALITY. Computed tomography reveals absence of the septum pellucidum (arrow), which may be associated with ONH
|
Presentation
The presenting visual acuity varies widely in ONH, from complete blindness to almost normal in approximately 10% of patients.7 Poor visual behavior may be noticed by the patient’s parents. Infants with severe, bilateral ONH may present with minimal or absent visual response and nystagmus. In asymmetric cases, ONH may manifest as strabismus in the first year of life.
Diagnosis
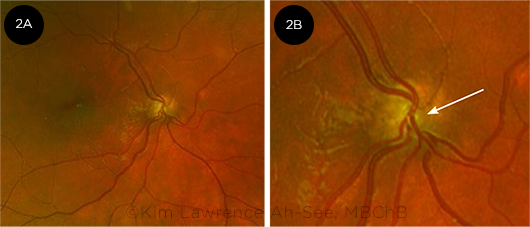
Clinical examination. ONH is primarily a clinical diagnosis based on identification of a small optic disc. On funduscopic examination of the optic nerve head, ONH can be easily recognized in severe or very asymmetric cases. The hypoplastic optic disc can be assessed by noting the caliber of the retinal vessels compared with those of the more normal disc in the fellow eye. The vessels may also show increased tortuosity and reduced branching patterns (Fig. 2A).5 In addition, there may be a peripapillary defect, and its choroidal edge may be pigmented, producing the so-called double-ring sign (Fig. 2B).
However, in milder cases, ONH may be more easily missed. The peripapillary defect can expose a rim of sclera, which may be mistaken for the normal optic disc rim or even for optic atrophy. Direct ophthalmoscopy and disc photography allow visualization of these features.
Differential diagnosis. The appearance of ONH should be distinguished from the following conditions:
- Optic nerve atrophy
- Tilted optic disc
- Glaucoma
In addition, severe bilateral cases of ONH may mimic achromatopsia or Leber congenital amaurosis.
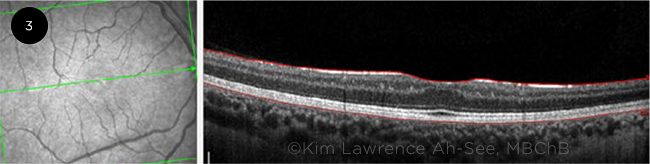
Imaging. OCT can be especially useful in identifying RNFL thinning in segmental ONH, which affects a portion of the nerve rather than the whole of it. However, eliciting cooperation from young children during the imaging process may be challenging. OCT can also demonstrate thinning of inner retinal layers when there is associated foveal hypoplasia (Fig. 3).
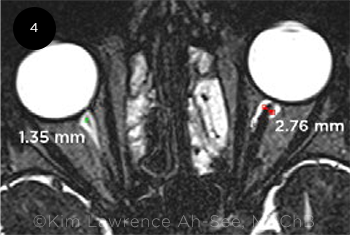
Magnetic resonance imaging (MRI) can demonstrate asymmetry of the caliber of the optic nerve in most moderate to severe cases (Fig. 4), and neuroimaging is indicated to exclude structural brain abnormalities.
Electrophysiology. In ONH patients, the electroretinogram and electro-oculogram results are normal, but visual evoked potentials are reduced. However, electrophysiologic testing is not routinely used in clinical practice.
 |
|
FUNDUS FINDINGS. (2A) Abnormal vascular configuration (reduced branching superonasally) in ONH. (2B) Double-ring sign with pigmented peripapillary defect (arrow).
|
Ocular and Systemic Associations
When ONH is diagnosed, it is of crucial importance to search for potential associated abnormalities. Ocular associations may include microphthalmos, aniridia, coloboma, and foveal hypoplasia.1
Systemic associations include hypothalamic dysfunction, which can produce pituitary, adrenal, or thyroid insufficiencies, especially in severe bilateral cases of ONH. These may manifest as disordered temperature regulation, hyperphagia and obesity, and disrupted sleep-wake cycles. These patients are also at significant risk of developmental delay, and an increased prevalence of autistic spectrum disorders has been reported among ONH patients.8
 |
|
FOVEAL HYPOPLASIA. OCT scan shows associated foveal hypoplasia in a patient with ipsilateral optic nerve hypoplasia.
|
Management
No specific treatments are available for ONH itself, but the patient’s outcomes can be improved with multidisciplinary management. As noted above, neuroimaging and investigation of the hypothalamic/pituitary axis are critical in identifying potentially life-threatening hormonal dysfunction.
Beyond making the early clinical diagnosis of ONH, the ophthalmologist has an important role in educating the family about this condition and making referrals to services and resources for children with significant visual disability. For example, timely mobility training, low vision aids, and specialized teaching support can optimize outcomes for patients with poor vision, as well as for those with associated neurodevelopmental delay and/or autism spectrum disorders.
Annual vision checks should be considered, and appropriate refractive correction provided. As in most patients, the burden of amblyopia treatment and strabismus surgery should be weighed against the visual potential of the affected eye.
Notably, some children experience improvement in their vision in the early years of life. It has been suggested that this improvement may be related to thyroid status,9 but this remains unclear. Other researchers attribute the visual improvement to the maturing of myelination in the young child.10
 |
|
UNEQUAL NERVES. MRI, axial view, demonstrates reduced caliber of the hypoplastic optic nerve (right eye) in unilateral ONH.
|
Conclusion
ONH is an important cause of visual impairment in infants and children. Although there are no treatments for ONH itself, the ophthalmologist’s early identification of this condition allows for prompt investigation of associated neuroendocrine disorders that can have a profound impact on the patient’s systemic health and may be amenable to timely intervention. Moreover, a multidisciplinary approach involving low vision resources and specialized training can help children with ONH achieve their potential.
__________________________
1 Garcia-Filion P, Borchert M. Curr Treat Options Neurol. 2013;15(1):78-89.
2 Lambert SR et al. Surv Ophthalmol. 1987;32(1):1-9.
3 Mohney BG et al. JAMA Ophthalmol. 2013;131(7):898-902.
4 Patel L et al. J Pediatr. 2006;148(1):85-88.
5 Dahl S et al. Acta Paediatr. 2018;107(3):484-489.
6 Borchert M, Garcia-Filion P. Curr Neurol Neurosci Rep. 2008;8:395-403.
7 Siatkowski RM et al. Ophthalmology. 1997;104(3):493-496.
8 Ek U et al. Acta Paediatr. 2005;94(10):1421-1426.
9 Fink C et al. J AAPOS. 2012;16(5):418-423.
10 Magoon EH, Robb RM. Arch Ophthalmol. 1981;99(4):655-659.
__________________________
Dr. Ah-See is an ophthalmology specialty registrar (resident) and Dr. Chan is a consultant ophthalmologist; both are at Princess Alexandra Eye Pavilion in Edinburgh, United Kingdom. Financial disclosures: None.
Write a Pearls article for EyeNet
Interested in sharing with your colleagues the latest evidence-based information about the diagnosis and medical and/or surgical management of a specific disease entity? If so, write an EyeNet Ophthalmic Pearls article. Articles typically offer step-by-step overviews of etiology, diagnosis, treatment, and follow-up. A checklist and writers guidelines are available at aao.org/eyenet/write-for-us.
|