Download PDF
Numerous studies have linked tooth loss resulting from periodontal disease to systemic conditions including diabetes, cardiovascular disease, rheumatoid arthritis, certain cancers, and neurodegenerative diseases. Now, we may consider adding primary open-angle glaucoma (POAG) to that list. A large prospective cohort study has found that recent tooth loss was associated with an increased risk of POAG.1
Tooth loss + gum disease = increased risk. Findings were based on data from the ongoing Health Professionals Follow-up Study, in which 40,536 men answered questions biennially about their health, including ocular and oral health status. Over a 26-year period, the researchers confirmed 485 cases of POAG through review of medical records. At each 2-year period within that span, they identified participants 40 years and older who reported eye examinations and were free of POAG.
Periodontal disease by itself was not associated with POAG, said Jae H. Kang, ScD, associate epidemiologist at Brigham and Women’s Hospital and assistant professor of medicine at Harvard Medical School. However, tooth loss in the past 2 years was associated with a 1.45-fold increased risk of POAG. And tooth loss accompanied by prevalent periodontal disease showed the strongest association: a 1.85-fold increased risk of POAG.
What’s the connection? The researchers theorize that oral infections, particularly those implicated in periodontal disease, trigger a cascade of events in which inflammatory microbes and their attendant cytokines originating in the vascular bed at the base of the tooth ultimately reach the optic nerve head microcirculatory system. The result: endothelial cell dysfunction that may compromise retinal ganglion cell axons.
Although the study looked only at men, Dr. Kang said that the findings likely would hold for women, since periodontal disease has been associated with systemic diseases in both sexes.
Dr. Kang urged caution in interpreting the results, saying that further study is needed. “One epidemiologic study cannot establish causal relations,” she said. “Nevertheless, this study’s findings raise the possibility that systemic adverse effects of poor oral health may also impact eye health.”
—Miriam Karmel
___________________________
1 Pasquale LR et al. Ophthalmology. 2016;123(11):2318-2327.
___________________________
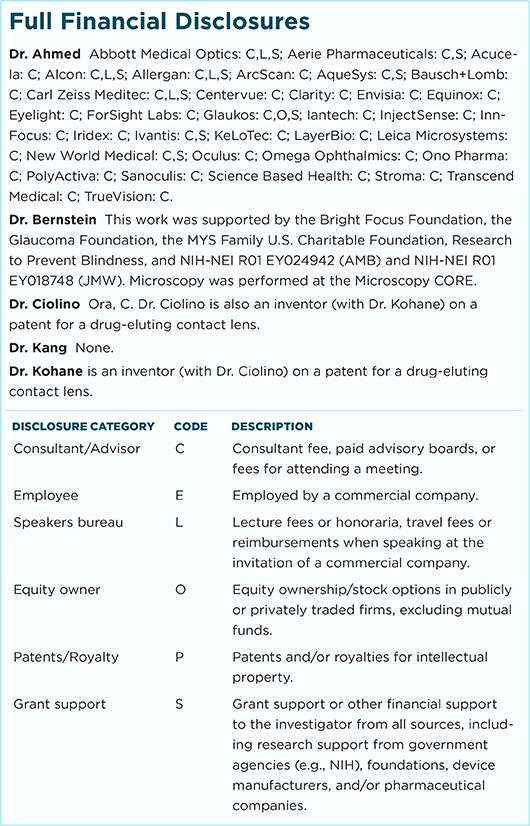
Relevant financial disclosures—Dr. Kang: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review