Download PDF
When it comes to surgical repair of orbital floor fractures, the consensus among oculoplastic specialists is that less is often more. Many fractures of the orbit, a common occurrence with facial trauma, never require surgery, which is customarily performed in patients with restricted motility, diplopia, and enophthalmos. And even if surgery is needed, there may be no rush. Sometimes waiting yields better outcomes.
“Not every orbital fracture needs to be repaired,” said Col. Raymond I. Cho, MD, FACS, with the Walter Reed National Military Medical Center and the Uniformed Services University of the Health Sciences. “Oculoplastic surgeons deal with all the complications resulting from orbital fracture repair. So it gives us greater pause to do surgery without strong indications,” he said. Some of these complications include the very things that surgery is intended to avoid: vision loss, double vision, globe malposition, hypoesthesia, and lid malposition.
“Even if nothing bad happens, the patient may have undergone surgery for no reason,” said Paul D. Langer, MD, FACS, at Rutgers New Jersey Medical School. “In a large majority of cases, it’s better to wait for a period of time after the injury.
“The issue is,” he continued, “which of these fractures need to be fixed, when do they need to be fixed, and in what time frame?” To help answer these questions, three oculoplastic specialists discuss their approach to making treatment decisions.
|
Assessing the Damage
|
 |
|
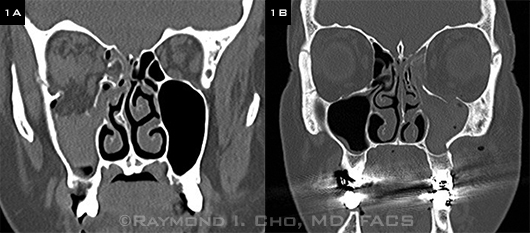
Orbital floor fractures, both involving more than 50 percent of the floor’s surface. (1A) With greater displacement and herniation of orbital contents, this fracture is much more likely than the other (1B) to cause enophthalmos.
|
Decisions Vary by Specialty
Dr. Langer said that the tendency among nonophthalmic physicians, who frequently assume care of trauma patients, is almost always to operate. “In many hospitals, ENT surgeons, plastic surgeons, and oral maxillofacial surgeons make up the majority of the facial trauma team. Their criteria for repair are much different from ours. Some will repair every fracture they see—and they’ll repair them immediately. The specialty, rather than the injury, may determine if and when surgery is performed.”
Fortunately, however, patients scheduled for orbital surgery are typically referred to an ophthalmologist to be sure the eye is uninjured, giving the Eye M.D. a chance to weigh in. “Frequently, I’ll call the surgeon and say, ‘In my opinion, this might be someone who might benefit from holding off,’” Dr. Langer said.
Urgent Treatment Needed
Even though surgical repair can be safely deferred in many patients, it’s essential to recognize situations in which timely treatment is needed. Muscle entrapment is one such scenario.
The white-eyed blowout, or trapdoor, fracture represents a small percentage of cases and occurs most often in children. Unlike the brittle bones of adults that break into pieces, children’s bones are malleable and break like green sticks (lending yet another name to the fracture). In such fractures, the bone tends to snap back into place and, in the process, entraps some muscle or orbital fat. Motility becomes so restricted that attempted eye movement results in severe pain, nausea, and possibly oculocardiac reflex, in which the heart rate slows down. Such cases require immediate surgery because the motility won’t improve over time, Dr. Langer said.
“It’s an emergency,” said Dr. Cho, “because if the muscle is left entrapped within a fracture, it can become ischemic, which may result in permanent diplopia.”
Vikram D. Durairaj, MD, FACS, at the University of Colorado, Denver, agreed. “Muscle entrapment or oculocardiac reflex are indications for immediate surgery. We operate within hours,” he said.
Diagnosing entrapment. The most common types of muscle entrapment involve the inferior rectus muscle in the case of a floor fracture, and the medial rectus in a medial wall fracture. Dr. Cho said that a clinical exam is needed to distinguish between entrapment and herniation. Although CT scans will reveal a fracture, they may not show whether a muscle is trapped.
Dr. Cho said that herniation of orbital contents into the sinus cavity can limit ocular motility, as can orbital edema resulting from the initial trauma. However, differences are apparent: “Typically, the degree of motility limitation is much worse with entrapment than with herniation.”
Sometimes, though not always, restriction will be worse in the direction of the muscle’s action than it is in the opposite direction, Dr. Cho said. For example, if the inferior rectus muscle is entrapped in a floor fracture, upgaze and downgaze restriction will occur. But, often, downgaze is more restricted. Pain may also occur with attempted upgaze or downgaze, and it is often worse when looking in the direction of the muscle being used.
A Tale of Two Patients
The downside of rushing in. Observation might have led to a different outcome for a young man who ended up in Dr. Cho’s office after multiple surgeries to treat injuries suffered in a car crash. The patient had a zygomaticomaxillary complex (ZMC) fracture with involvement of the orbital floor, which had been repaired by the referring service (not an oculoplastic surgeon). After the initial surgery, the patient had diplopia, hyperglobus, and cicatricial entropion (Fig. 2). Finally, after attempting two revisions, the surgeon referred the patient to Dr. Cho, who determined that the patient probably had not needed the orbital floor fracture repair in the first place. “The orbital complications could have been entirely avoided,” he said.
The upside of waiting. Dr. Langer may have saved a different patient from a similar fate when he was called in for a routine consultation on a teenager who was injured in a car crash. After finding that the patient’s eye movements were fine and the fracture was small, Dr. Langer told the patient that he might not need surgery, which would involve taking a bone graft from the iliac crest and shaping it to fit into an incision through the eyelid. But the patient’s father insisted that they follow the referring surgeon’s recommendation. Dr. Langer offered to speak with the surgeon. Then hospital transport arrived to take the patient to the OR. Dr. Langer did speak with the surgeon, who canceled the operation. Two weeks later, when Dr. Langer followed up with the patient, his eye and ocular motility were fine. “If I had seen him an hour later, he would have undergone surgery. That is not uncommon. He didn’t need surgery at all.”
 |
|
Unnecessary Surgical Complications. This patient was referred to Dr. Cho following ZMC/orbital floor fracture repair and two attempted revisions. (2A) At presentation: Note significant hyperglobus and lid/lateral canthal malposition. (2B) Postoperative photograph following orbital fracture revision, midface lift, and lateral canthopexy.
|
|
Watchful Waiting
With the exception of muscle entrapment or oculocardiac reflex, Dr. Durairaj delays surgery to allow swelling to go down. The delay also allows for the proper coordination of surgical care, which is difficult in an emergency repair situation.
In the early stages after an injury, said Dr. Langer, it’s hard to determine the cause of restricted motility: Is it from the fracture itself or from swelling? “The only way to be sure is to follow the patient as the swelling resolves.” He said the worst potential outcome of operating early is compartment syndrome, a potentially blinding condition in which excessive swelling and edema compress the optic nerve. It’s a rare occurrence, but the risk is greater when surgery is performed in a swollen orbit.
How long to wait. Though the consensus among oculoplastic surgeons is that watchful waiting is often appropriate, there is some debate over the length of the observation period. Some advocate intervention within the first two weeks of injury, while others suggest waiting up to six months.1
Some orbital surgeons worry that postinjury scarring, which can occur during a wait of several weeks, may make dissection and repair more difficult if surgery is deferred, Dr. Cho said. However, he added, “My experience is that scarring, if not too extreme, should not significantly impact the outcome of surgery. A good surgeon should be able to deal with it.”
Is two weeks the sweet spot? Two weeks is sometimes considered a benchmark, he continued, because it strikes a balance between allowing edema to resolve and avoiding excessive scarring. Dr. Cho is more likely to repair within a two-week window if there’s a very large fracture with a high likelihood of enophthalmos or significant diplopia in primary gaze.
In contrast, Dr. Durairaj prefers to operate within five to seven days. “I feel that most of the swelling has resolved in a week, and if it is necessary to reduce the fracture, the bone is still easily repositioned.”
Dr. Langer said that there are no hard data to support surgery within a two-week window. “The only time I repair an isolated floor fracture early is when ocular motility is severely restricted.” If the eye moves a significant amount, he waits.
Unless there are contraindications, he puts the patient on oral steroids for three to five days to reduce the swelling. Then he examines the patient weekly, looking for improvement in motility by measuring the prism diopters (PD) of deviation. “For example, if a patient presents initially with a 20-PD hypotropia in upgaze, and one week later the deviation in upgaze is only 10 PD, that’s objective evidence that motility is improving, and good reason to follow the patient for another week,” he said.
The diplopia factor. Some doctors operate out of concern that diplopia, which often occurs immediately after trauma, will not improve if treatment is delayed too long. But Dr. Langer said that the double vision may resolve on its own. “If you can wait it out a couple of weeks, many patients who present with double vision will eventually have resolution of their diplopia. If the diplopia doesn’t resolve, and it interferes with the patient’s daily activities, then surgery is warranted.”
A frequently cited study by Dal Canto and Linberg2 demonstrated that patients fared equally well if their orbital floor fractures were repaired within 14 days or within 29 days after trauma. In this retrospective study of 58 patients, 36 eyes repaired within 14 days (mean of 9 days) were compared with 22 eyes repaired at up to 29 days (mean of 19 days). The authors found no statistical difference in postoperative binocular diplopia. However, they acknowledged that delayed repair may be more technically challenging. And, further, these results do not apply to white-eyed blowout fractures.\
Dr. Cho said that he agreed with Dal Canto and Linberg’s conclusions on diplopia outcomes. “I am much more likely these days to wait. A patient with a moderately sized floor fracture who has diplopia outside primary gaze—I will be more likely to observe for a few weeks. Often, their diplopia will resolve and they may not develop enophthalmos.”
Enophthalmos: a personal decision. A common practice has been to surgically repair an eye that is recessed 2 mm or more, Dr. Langer said. Delaying the intervention has advantages, since it takes awhile for the eye to sink, and most studies show that waiting doesn’t matter in terms of the ultimate surgical outcome.
He added that it’s difficult to predict a patient’s reaction to enophthalmos. “I allow enophthalmos to develop. If the patient doesn’t mind the way it looks, we can leave it,” Dr. Langer said. “I leave the decision to the patient, not to the numbers.”
Dr. Cho also disregards “the 2-mm rule.” “What matters to me is how the patient feels about how they look. I have patients with 3 or 4 mm [of recession], and they don’t care. On the other hand, some patients are very attuned to how they look, and they will notice 2 mm or sometimes even less.”
Fracture size. Some surgeons say that 50 percent involvement of the orbital floor or wall is an indication for surgery, Dr. Cho noted. “In my view, that’s a rather arbitrary measurement.” (For example, see the two fractures in Fig. 1). He prefers to measure the size of the fracture in two dimensions and the degree of fragment displacement on CT scan, then calculate the volume of orbital expansion using the formula for an ellipsoid. The ratio of volume expansion (in cc) to the expected amount of enophthalmos (in mm) is roughly 1:1. “So if the calculated volume is greater than 2 cc, I may watch them more closely or recommend earlier repair.”
Bottom line. “Nobody knows the number of patients who won’t need surgery,” Dr. Cho said. “But if the ophthalmologist recognizes that a fracture is small and has a low risk of enophthalmos and there’s not significant diplopia, then it’s desirable to recommend observation.”
___________________________
Raymond I. Cho, MD, FACS, is Director of Oculoplastic & Orbital Surgery Service, Walter Reed National Military Medical Center, and associate professor of surgery at the Uniformed Services University of the Health Sciences, in Bethesda, Md. Financial disclosure: None.
Vikram D. Durairaj, MD, FACS, is professor of ophthalmology and otolaryngology/head and neck surgery at University of Colorado, Denver. Financial disclosure: Is a consultant for Stryker and is on the speakers bureau for KLS Martin and AO Foundation.
Paul D. Langer, MD, FACS, is associate professor of ophthalmology and director, Division of Ophthalmic Plastic and Reconstructive Surgery, Institute of Ophthalmology and Visual Sciences, Rutgers New Jersey Medical School, Newark, N.J. Financial disclosure: None.
___________________________
1 Pelton RW. Management of orbital trauma. Focal Points. 2013;31(1):module 1.
2 Dal Canto AJ, Linberg JV. Ophthal Plast Reconstr Surg. 2008;24(6):437-443.