Download PDF
This month, News in Review highlights selected papers from the original papers sessions at AAO 2021. Each was chosen by the session chairs because it presents important news or illustrates a trend in the field. Only four subspecialties are included here; papers sessions also will be held in five other fields. For up-to-date information, check the Mobile Meeting Guide (aao.org/mobile).
What’s the best surgical strategy for managing medically uncontrolled glaucoma in patients who have not previously undergone incisional ocular surgery? According to the five-year findings of the Primary Tube Versus Trabeculectomy (PTVT) Study, both tube shunts and trabeculectomy with mitomycin C (MMC) are viable surgical options.
Same—but different? “The PTVT Study does not demonstrate clear superiority of one glaucoma operation over the other,” said Steven J. Gedde, MD, at Bascom Palmer Eye Institute in Miami and a study chairman.
Even so, the data suggest that the choice is more than a flip of the coin for some patients. For instance, those patients with lower preoperative IOP appear to benefit most from primary trabeculectomy with MMC, while those with higher pre-op IOP may benefit more from primary tube shunt surgery. “Before seeing the results of the PTVT Study, I was unaware of the importance of preoperative IOP when selecting a traditional glaucoma procedure,” Dr. Gedde said.
In addition, the results for trabeculectomy with MMC were achieved with significantly fewer glaucoma medications, a finding that could influence treatment decisions.
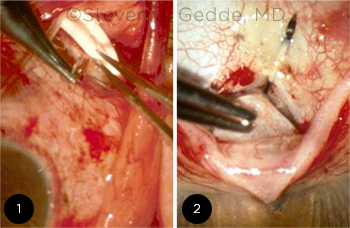 |
NO CLEAR WINNER. Although results were similar for tube shunt surgery (1) and trabeculectomy (2), nuances from the PTVT Study may influence treatment decisions for selected patients.
|
Study specifics. For this multicenter randomized clinical trial, patients with medically uncontrolled glaucoma were randomly assigned to treatment with a 350-mm2 Baerveldt shunt (Johnson & Johnson) or trabeculectomy with MMC (0.4 mg/mL for two minutes). Primary outcome measures included rate of surgical failure defined as IOP >21 mm Hg or reduced <20% below baseline; IOP≤ 5 mm Hg; repeat glaucoma surgery; or loss of light perception vision.
Outcomes. At the five-year follow-up, mean IOP was similar for both procedures (13.4 mm Hg for the tube group vs. 13.0 mm Hg for trabeculectomy; p = 0.52). What’s more, the cumulative probability of failure was not significantly different between the tube and trabeculectomy cohorts (42% vs. 35%, respectively; p = 0.21).
With regard to the need for supplemental medications, the rate of complete success without additional medications was higher for patients in the trabeculectomy plus MMC group (34%) than for those who received the shunt (9%; p < .001).
A surprise finding. At the one-year follow-up, the surgical failure rate was significantly higher in the tube group (17%) than in those who underwent trabeculectomy (8%). But by the end of five years, the difference was no longer statistically significant.
A risk factor analysis found lower preoperative IOP to be significantly associated with failure. Specifically, the rate of tube shunt failure was strongly influenced—and trabeculectomy failure was less influenced—by pre-op IOP, Dr. Gedde said.
Bottom line. While both procedures are viable surgical options for managing refractory glaucoma, the findings suggest that trabeculectomy with MMC is the preferred surgical procedure in the subgroup of patients who either are nonadherent or are poorly tolerant of glaucoma therapy, said Dr. Gedde. He added, “Surgical skill and experience with each operation are important additional considerations that were not evaluated in this study.”
—Miriam Karmel
|
Treatment Outcomes in the Primary Tube Versus Trabeculectomy Study After 5 Years of Follow-Up. Presented during the first glaucoma original papers session. When: Saturday, Nov. 13, at 8:48 a.m. Where: Room 255-257.
|
___________________________
Relevant financial disclosures—Dr. Gedde: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Chang AcuFocus: S; Allergan: C,L,S; Carl Zeiss Meditec: C,L,S; Johnson & Johnson Vision: C,L,S; Omega Ophthalmics: C,O.
Dr. Gedde None.
Dr. Uddaraju None.
Dr. Wieland Roche: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|
More from this month’s News in Review