By Lori Baker-Schena, MBA, EdD, interviewing Robert A. Goldberg, MD, Femida Kherani, MD, and Rachna Murthy, MBBS, FRCOphth
Download PDF
While dermal fillers have come a long way since the days of paraffin wax and fat injections to improve facial function and aesthetics, the periocular hyaluronic acid (HA) dermal fillers of today are not without their complications.
Fortunately, most adverse reactions are transient and mild, noted Robert A. Goldberg, MD, at the UCLA Stein Eye Institute in Los Angeles. Yet the rarer complications—such as skin necrosis, blindness, and stroke—can be catastrophic, “which is why we encourage clinicians to become familiar with managing the range of complications.”
The need for education is particularly pressing given the popularity of HA fillers, which were first FDA-approved in 1996 and today represent a multibillion-dollar industry.
Many nonophthalmologists inject these fillers, including dermatologists, plastic surgeons, and dentists. (See “In Whose Hands?”) But if there is a vision-related complication, ophthalmologists may be called upon in the management, said Femida Kherani, MD, at the University of British Columbia in Vancouver, British Columbia, Canada.
“These injectors will call the ophthalmologist first if there is an issue,” Dr. Goldberg agreed. “Consequently, more and more ophthalmologists are finding themselves on the front lines treating complications, and thus it is imperative that they have a basic understanding of possible side effects.”
 |
|
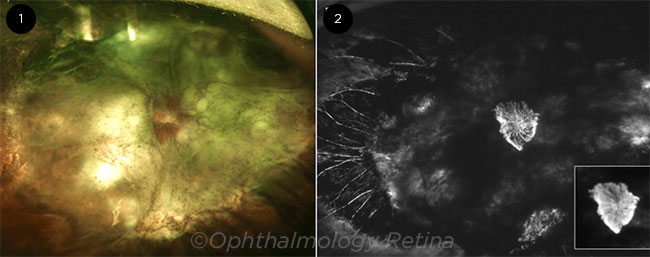
ADVERSE OUTCOME. This 26-year-old patient lost vision eight minutes after an injection of a dermal filler. (1) Funduscopy revealed neovascularization of the optic disc and an extensive retinal detachment. (2) Widefield fluorescein angiography showed leakage from the neovascularization (see inset) and nonperfusion of the retinal vasculature.
|
Why HA Fillers Are Popular
HA dermal fillers revolutionized the market seemingly overnight, thanks to their good safety profile and the fact that they are reversible, said Rachna Murthy, MBBS, FRCOphth, at Cambridge University Hospital in Cambridge, United Kingdom.
“Because hyaluronic acid is a naturally occurring linear polymeric dimer of N-acetylglucosamine and glucuronic acid, which is a component of all connective tissue in living beings, the [overall] risk of immunological rejection is low,” Dr. Murthy pointed out.
Moreover, while HA fillers are biodegradable, “their duration can last from six to 24 months or even several years in the periocular area,” Dr. Murthy said.
Another advantage: HA fillers, which are available in a range of viscosities, are dissolvable. “If you have a complication, you have an opportunity to dissolve the product using hyaluronidase,” Dr. Kherani said. “Here is an example: A patient schedules a blepharoplasty consult, presenting with a nodule or asymmetry. If the problem is related to a previous hyaluronic acid injection, the patient can be easily treated with hyaluronidase agents and subsequent blepharoplasty, as needed.”
Overview of Indications
Aesthetic. HA fillers are commonly used for purely cosmetic reasons. But they also can be used “to improve the aesthetics in reconstructive cases such as facial palsies, postcancer defects, and trauma cases,” said Dr. Kherani. Moreover, she said, they can be combined with neuromodulators such as botulinum toxin (Botox).
Functional. HA fillers can serve as a viable nonsurgical alternative for some functional disorders as well as a temporary treatment until surgery can be performed, Dr. Murthy said.
These products have been used for myomodulation, in which muscle function is altered by placing filler in the tissue planes—thus altering the fulcrum of a muscle as well as augmenting or reducing its strength.1 “I use hyaluronic acid fillers on my facial palsy patients,” Dr. Murthy added, “as this helps with muscle strength.”
A note on quality of life. Dr. Murthy also stressed that these fillers can have a beneficial impact on quality of life. “The role of appearance in a patient’s quality of life cannot be emphasized enough,” she said. “For example, we need to give skin cancer patients whose surgery left them with facial defects the best cosmetic outcomes.”
In another example, she cited patients with thyroid eye disease. “We can treat the double vision and optic neuropathy associated with active thyroid eye disease, but we can’t offer these patients surgery for their appearance,” Dr. Murthy said. “Dermal fillers can serve as a treatment alternative, especially when the eye disease is active, and help improve their quality of life.”
In Whose Hands?
Unfortunately, “Not everyone who is injecting fillers has the sophisticated understanding of what can happen to the visual system if the injection is done incorrectly,” Dr. Goldberg said.
At the 2019 Oculofacial Plastic Surgery Subspecialty Day, Dr. Murthy issued a challenge to the audience: Ophthalmologists should not only manage the complications referred to them but also step up and actually do the treatments. “While we often see facial plastic surgeons and dermatologists offering dermal fillers to their patients, both oculofacial plastic surgeons and general ophthalmologists should be more actively providing this treatment,” she said.
|
Potential Complications
As the numbers of minimally invasive cosmetic procedures performed in the United States increase each year, the rates of filler complications have also increased.2,3
Mild. Most complications are mild: More than 90% of adverse outcomes related to HA fillers involve redness, swelling, or bruising at the injection site.1 Other mild complications include early-onset nodules as a result of accumulation of filler in one area.
Another complication of note in the periocular area is blue-gray dyschromia, also known as the Tyndall effect. This can result from overly superficial placement or large boluses of the HA filler. The use of too viscous a product has also been implicated.1 Fortunately, the blue-gray discoloration can be managed with cover makeup, and the filler can be dispersed with hyaluronidase.
Inflammatory. Inflammatory nodules associated with HA filler are triggered by the immune system, even by something as simple as a respiratory infection, Dr. Murthy said. These complications can be treated with antibiotics for the triggering infection.
Dr. Murthy also warned of the risk of delayed complications from HA products, including delayed-onset nodules, which can appear years after treatment in the periocular area. “Hyaluronic acid fillers were originally thought to be nonimmunogenic,” she said. However, as clinicians learn more about the immune system and the fillers, they are finding that an immune response can be triggered by something as basic as a tooth extraction or a cold, she said. Dr. Murthy added, “This is why a thorough history is so essential when managing these patients: They could have had the dermal filler procedure years before.”
Serious. In 2015, 98 cases of blindness due to fillers were documented in the literature. Of these, 23.5% were associated with HA fillers.4 The authors updated these statistics through 2018, adding 48 new published cases of vision loss after injection of a filler.5 An HA filler was the cause of these complications in 81.3% of cases, with vision loss, pain, ophthalmoplegia, and ptosis the most common reported symptoms.
Vision loss. Historically, 190 cases of blindness due to aesthetic injectional treatments have been reported in the literature from 1906 to 2019,1 a statistic Dr. Murthy said may be underreported. In her review article, she noted that the periocular area such as the glabella, injected for the treatment of frown lines, and the dorsum of the nose during nonsurgical rhinoplasty are the most common areas responsible for vision loss. Hyaluronic acid, with its smaller particulate size, is more likely to obstruct the distal branches of the ophthalmic artery.
Managing Complications
Even though vascular occlusions resulting in skin necrosis, cerebrovascular infarction, and intracranial emboli are relatively rare, it is important for those who inject dermal fillers to understand how to manage potential complications, Dr. Goldberg said.
For example, flooding the tissue with high-dose hyaluronidase until reperfusion is obtained can reverse skin necrosis.1 Yet the ability of retrobulbar hyaluronidase to reverse vision loss remains unclear. “There is only a handful of reported cases of retrobulbar hyaluronidase being effective, with no well-documented case of vision returning from an embolism,” Dr. Goldberg noted. “And even when someone attempts retrobulbar hyaluronidase, we have to recognize that based on current data, it is a heroic attempt, like throwing a ‘Hail Mary’ pass, but still very unpredictable in terms of success.”
Dr. Goldberg noted that the controversy surrounding retrobulbar hyaluronidase falls into two schools of thought: Some clinicians feel that this approach is state-of-the-art treatment, while others believe that the danger of retrobulbar injections given by nonexpert hands is higher than the likelihood of improvement.
Minimizing Risk
Dr. Goldberg stressed that no clear evidence-based guidelines exist on how to prevent or eliminate filler complications. “Even the worst complications happen to the best injectors, and there is no way to get the complication incidence to zero,” he said.
Having said that, he added, there are several ways to reduce the risk of complications. Among them:
- Be able to identify the safe planes in which to inject the filler, and avoid the areas known to have major vessels that communicate with the orbit.
- Inject HA fillers slowly and precisely. Dr. Kherani also recommended injecting small amounts—0.1 cc—at a time.
- Understand the difference between various fillers. “It is vital to be familiar with the various fillers to determine the best product for the desired outcome, as well as the different HA concentrations and optimal depth of placement,” Dr. Murthy said.
- Select patients carefully. “A thorough medical, surgical, and aesthetic history is important prior to treatment,” Dr. Murthy emphasized.
___________________________
1 Murthy R et al. Curr Opin Ophthalmol. 2019;30(5):395-400.
2 Ortiz AE et al. Dermatol Surg. Published online Oct. 11, 2019.
3 Heydenrych I et al. Clin Cosmet Investig Dermatol. 2018;11:603-611.
4 Beleznay K et al. Dermatol Surg. 2015;41(10):1097-1117.
5 Beleznay K et al. Aesthet Surg J. 2019;39(6):662-674.
___________________________
Dr. Goldberg is an oculoplastic surgeon at UCLA Stein Eye Institute in Los Angeles. Financial disclosures: None.
Dr. Kherani is an oculoplastic surgeon and on the clinical faculty at the University of British Columbia in Vancouver, British Columbia, Canada. She is also with the Heights Laser Center in Vancouver and on the clinical faculty at the University of Calgary in Calgary, Alberta, Canada. Financial disclosures: Allergan: L; Merz: L; Novartis: L.
Dr. Murthy is an oculoplastic surgeon at Cambridge University Hospital in Cambridge, United Kingdom, where she directs the Thyroid Eye Disease Service. She is also director of Advanced Plastic & Aesthetic Consultants in Newmarket, United Kingdom. Financial disclosures: Allergan UK: C.
See the disclosure key at www.aao.org/eyenet/disclosures.