By Lisa Chung, Andrew Jilwan, and Gerald G. Striph, MD
Edited by Steven J. Gedde, MD
Download PDF
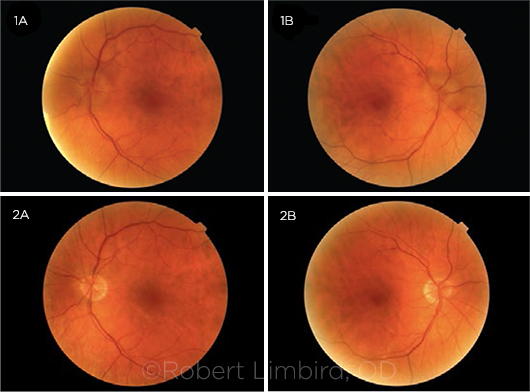
At 65 years old, Adam Ribley* had few health problems and visited his optometrist only for routine checkups. Color fundus photos were taken at each visit. At one appointment, the optometrist was surprised to see that the optic discs were congested, in stark contrast to 2 years previously. He diagnosed Mr. Ribley with bilateral disc edema and set up a neurology appointment for him.
Neurology Workup
History and physical. The neurologist learned that Mr. Ribley had smoked years ago but had no recent medical problems other than a “mild flu” that had resolved months previously. Mr. Ribley denied headaches, vision changes, and tinnitus, and he had a normal neurologic examination. In short, his medical history was unremarkable.
Lab work and imaging. Complete blood count, erythrocyte sedimentation rate, and C-reactive protein were normal. Because the funduscopic exam suggested intracranial hypertension, magnetic resonance imaging (MRI) with contrast was performed on the brain. The MRI was negative for intracranial lesions, and the optic nerves looked normal. Neurology then ordered a lumbar puncture (LP).
We Get a Look
Neurology sent Mr. Ribley to us for a neuro-ophthalmology exam. The ophthalmic exam was unrevealing, with the exception of funduscopy. The patient’s best-corrected visual acuity was 20/20 in both eyes, Humphrey visual fields were normal, there was no afferent pupillary defect (APD), and there were no motility problems. Intraocular pressure measured 18 mm Hg in the right eye and 16 mm Hg in the left. Funduscopic exam showed bilateral mild disc edema. The appearance seemed consistent with true papilledema, inflammation, or an infiltrative-type picture. In our opinion, his previous MRI and follow-up fluorescein angiogram (FA) were unremarkable. At 1 and 2 months after the initial visit, Mr. Ribley’s funduscopic exam remained unchanged despite trials of Diamox (acetazolamide) and oral steroids.
Meanwhile, LP results were within normal limits except for mildly elevated protein (opening pressure, 10 cm H2O; total protein, 63 mg/dL; glucose, 58% of serum glucose; and 1 red blood cell/1 white blood cell [5 lymphocytes, 5 macrophages, 1 segmented neutrophil]).
Differential Diagnosis
At this point, our differential included the following.
Intracranial hypertension. Increased intracranial pressure (ICP) can cause bilateral optic disc edema. Possible etiologies include intracranial tumors, hemorrhage, and venous sinus thrombosis. The patient presented with what initially appeared to be papilledema; however, the unremarkable MRI, lack of leakage on FA, and normal cerebrospinal fluid (CSF) opening pressure greatly decreased the likelihood of these causes.
Infectious diseases. Infections can cause optic disc edema through inflammation or immune-mediated processes in response to the pathogen. In Mr. Ribley’s case, this was investigated by CSF analysis, which included testing for herpes simplex virus, JC virus (a member of the Polyomaviridae family), fungal cultures, West Nile virus, and varicella-zoster virus, as well as acid-fast stain, Venereal Disease Research Laboratory test, and Lyme titer—all of which were negative.
Medication. An array of medications are associated with optic neuropathy, including—but not limited to—amiodarone, sildenafil, and infliximab. However, a review of our patient’s medications ruled out a pharmacologic etiology.
Other. Other etiologies that cause bilateral optic disc edema are infiltrative processes such as sarcoidosis, amyloidosis, and multiple myeloma. These diseases may lead to elevated protein in CSF, and they do not always cause optic nerve dysfunction despite causing edema.
Sarcoidosis can manifest initially with ocular signs, the most common being uveitis. However, it can also cause optic neuropathy without uveitis. Most patients with neurosarcoidosis have an elevated angiotensin-converting enzyme level and an abnormal brain MRI, but our patient did not.
Amyloidosis can affect the eye as part of systemic disease or present locally. Involvement of the optic nerve is usually by local extension of surrounding disease, which was not visible in our patient.
Multiple myeloma is marked by overproduction of immunoglobulins and can affect the entire body. Abnormal proteins can also come from tumors remote from the eye.
Making the Diagnosis
Because of the slightly abnormal CSF protein results, a repeat brain MRI and LP with cytology were performed. Once again, MRI was unremarkable. The repeat LP showed normal opening pressure, but total protein was now significantly elevated. For this reason, serum protein electrophoresis was done.
The LP results showed mild hypogammaglobulinemia, 0.6 (normal, 0.69-1.41); small extra protein band, 0.15 g/dL in the gamma region; immunofixation, monoclonal IgA lambda protein in gamma region; actual IgA level was normal with a value of 213; and IgG and IgM were mildly low.
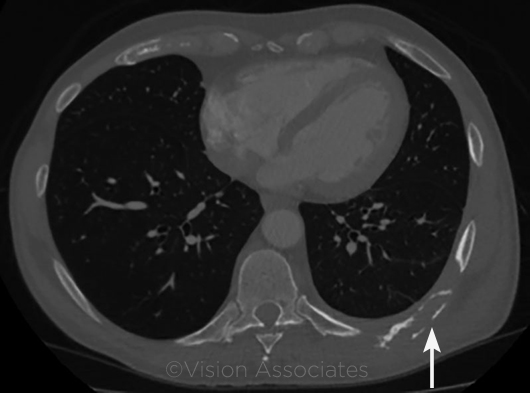
A search for the source of the lambda spike was done with computed tomography (CT) of the chest and pelvis. The CT revealed a single lytic lesion of the posterior ninth left rib. Subsequent PET scan confirmed that the solitary lesion was highly active and destructive. Based on biopsy of the lesion, we diagnosed Mr. Ribley with a plasmacytoma.
 |
|
CT. The patient had a single lytic lesion (arrow) of his ninth left rib.
|
Patient Course
Mr. Ribley returned for follow-up regularly throughout the course of diagnosis and treatment. The lytic lesion was treated with radiation therapy by oncology, which determined that systemic therapy was not indicated. One month after Mr. Ribley started treatment, the appearance of his optic disc began normalizing. After 8 months and completion of the course of radiation, his discs looked much as they had in the optometrist’s baseline photos from several years ago.
This recovery confirmed that the plasmacytoma had caused the infiltrative optic neuropathy.
 |
|
CONGESTED DISCS. During a routine checkup, funduscopy (Figs. 1A, 1B) revealed a big change from what the optometrist had seen 2 years previously (Figs. 2A, 2B).
|
Discussion
Plasmacytomas are a neoplastic proliferation of a single plasma cell. They are normally located in bone marrow and are found twice as often in men than women. Patients are typically between the ages of 55 and 60 when the diagnosis is made.
Presentation. They can present as single lesions called plasmacytomas or as multiple lesions in multiple myeloma (MM). Plasma cell tumors cause various symptoms depending on their location, but they very rarely cause optic disc changes unless a lesion is intracranial. Infiltrative ophthalmopathy without bilateral visual changes is rare, but it has been reported in the related condition, MM. The optic disc changes are likely caused by infiltration of the disc by neoplastic cells.1
A similar case. Plasmacytoma can cause optic disc edema through elevated ICP. While this is most commonly associated with intracranial lesions, a 2016 article by Grixti et al. described a 41-year-old patient who had a plasmacytoma outside the skull.1 He presented with a 9-month history of subjective decrease in vision. His visual exam was normal except for reduced color vision; he could correctly identify only 6 of 17 isochromatic Ishihara plates. Funduscopic exam revealed bilateral disc swelling. Brain MRI was unrevealing, and an LP showed a normal opening pressure (19 mm Hg) with a significant increase in CSF protein. An eventual spinal MRI revealed a tumor of the T9 vertebral body. Radiotherapy greatly improved disc edema, with complete resolution 8 months after treatment. Despite the normal opening pressure on LP, Grixti et al. believe that the disc edema was due to increased ICP. Their reasoning is that the pressure was increased rostral to the T9 tumor but reduced caudally. Radiotherapy reduced the tumor size and restored CSF flow, eventually leading to resolution of the papilledema.
Diagnosis. Diagnostic suspicion of plasmacytoma usually begins incidentally following a blood screen. Investigation in up to one-third of patients begins following pathologic fracture. Serum protein electrophoresis showing monoclonal light chain protein expansion can be a helpful clue. If the location of the mass is suspected in the spine or pelvis, CT/PET scans can elucidate their location. If the mass location is head or neck, MRI is preferred. Definitive diagnosis of plasmacytoma is made on the basis of biopsy results showing clonal plasma cell expansion.
Treatment. Treatment for plasmacytoma is radiation therapy with 40 to 50 Gy dosage or surgical resection if there is bone instability or compression of adjacent structures. Adjuvant chemotherapy is sometimes required. Prognosis is generally good, with median survival about 10 years after diagnosis. Retrospective studies found that 54% of people diagnosed with plasmacytoma progress to MM.
Our patient. Mr. Ribley’s case was unique; he had bilateral optic nerve involvement without any visual dysfunction from a solitary remote tumor. At 36 months, Mr. Ribley has not had a recurrence.
___________________________
* Patient name is fictitious.
___________________________
1 Grixti A et al. Eur J Ophthalmol. 2016;26(2):e32-e34. doi: 10.5301/ejo.5000701.
___________________________
Ms. Chung and Mr. Jilwan are fourth-year medical students at Toledo College of Medicine in Toledo, Ohio. Dr. Striph is in private practice in Toledo, Ohio. Relevant financial disclosures: None.