Sleep Apnea and Retinopathy
By Lynda Seminara
Selected By: Richard K. Parrish II, MD
Journal Highlights
American Journal of Ophthalmology, October 2017
Download PDF
Obstructive sleep apnea (OSA) is linked to ocular conditions caused by vascular dysregulation, including optic disc edema and nonarteritic anterior ischemic optic neuropathy. Advances in retinal imaging have enabled noninvasive accurate detection of retinal microvascular pathology, which may long precede clinical evidence of disease. Tong et al. examined the quantitative relationship between both static and dynamic retinal vascular caliber and the severity of OSA and found an independent association between retinal arteriolar narrowing and attenuated vascular pulsation amplitude.
For this prospective cross-sectional study, the researchers performed a quantitative analysis of retinal vascular caliber among patients with OSA, who were recruited from adult patients who planned to undergo diagnostic polysomnography at a private tertiary sleep unit in Australia. OSA severity was defined by the apnea-hypopnea index (AHI), as follows: ≥ 30 = severe; ≥ 15 to < 30 = moderate; ≥ 5 to < 15 = mild; and < 5 = control. Of the 115 final participants (mean age, 58 years; 73 males), OSA was severe in 41, moderate in 35, and mild in 25; the remaining 14 patients served as controls.
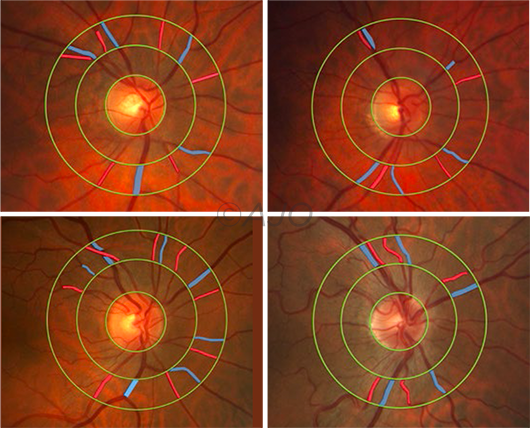 |
INCREASING SEVERITY. In this group of male patients, changes similar to mild hypertensive retinopathy became more apparent with increasing OSA severity. (Top left) No OSA; the patient’s apnea-hyponea index (AHI) was 3.0 per hour. (Top right) This patient had mild OSA and an AHI of 14.4/hr. (Bottom left) An example of moderate OSA; the patient’s AHI was 21.4/hr. (Bottom right) An example of severe OSA; the patient’s AHI was 40.6/hr.
|
Static retinal vascular caliber was calculated as the average diameter of retinal arterioles and venules and summarized as the arteriovenous ratio (AVR). Dynamic retinal vascular caliber was defined as the average pulsation amplitude of retinal arterioles and venules. Groups were compared using multivariate linear regression analysis. Results were adjusted for age, body mass index, and arterial pressure.
Increasing AHI was significantly associated with decreasing AVR and decreasing central retinal arteriolar equivalent. Also significant was the relationship between increasing AHI and attenuated retinal vascular pulsation amplitude. Qualitative grading of fundus photographs demonstrated that retinal vascular changes resembling mild hypertensive retinopathy were more common in patients with moderate and severe OSA than in controls.
The investigators concluded that OSA severity is independently associated with retinal arteriolar narrowing and attenuated vascular pulsation amplitude. Retinal vasculature is easily imaged and may be a surrogate biomarker of cerebral and systemic vascular risk in patients with OSA requiring extensive evaluation.
The original article can be found here.