By Lori Baker-Schena, MBA, EdD, Contributing Writer, interviewing Jon G. Dishler, MD, John F. Doane, MD, and Jason E. Stahl, MD
Download PDF
Small incision lenticule extraction, or SMILE, became clinically available as an alternative to LASIK in Europe and Asia in 2012. In September 2016, it was approved for the treatment of spherical myopia by the U.S. Food and Drug Administration (FDA). To date, more than 1 million SMILE procedures have been performed worldwide.1
During SMILE, the refractive surgeon uses a femtosecond (FS) laser to create a corneal lenticule, which is removed through a small incision—thus eliminating the need for one of the most iconic features of LASIK: the corneal flap.
Slow Adoption?
“In describing the advent of minimally invasive SMILE relative to LASIK, ophthalmologists have used the comparison of arthroscopic surgery versus open surgery,” said Jon G. Dishler, MD, who practices in the Denver area. He noted that, as in other areas of medicine, this represents a significant step forward.
Despite this apparent advantage, SMILE has experienced a slow start in the United States, Dr. Dishler acknowledged. He attributed this to the fact that U.S. approval officially covers the correction of spherical myopia only between –1 D and –8 D in eyes with –0.5 D or less of astigmatism. Elsewhere, those parameters are broader, encompassing up to –10 D of myopia and up to –6 D of astigmatism. (Dr. Dishler noted that treatment in the United States can take place up to –10 D, though a pop-up warning will occur.) In addition, at present, only the VisuMax (Carl Zeiss Meditec) is used for SMILE.
Moreover, “as with any new technology, there is usually a period of time during which adoption takes place, and there are new skills that surgeons must learn,” Dr. Dishler said (see “Challenges and Pearls,” below). “This is probably one of the most important factors” with regard to acceptance, he said.
 |
|
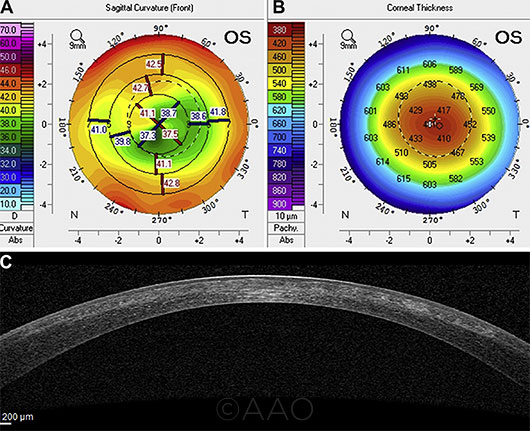
LEARNING CURVE. In an early study of outcomes, retreatment was needed in 7 cases, 6 of which were successful. However, the seventh retreatment produced irregular corneal topography (A, B) and a highly irregular corneal profile in the anterior stroma and a poorly defined SMILE interface (C).5
|
Benefits
FDA approval for compound myopic astigmatism is anticipated to take place this year, and other FS laser platforms are reportedly being adapted for SMILE.2 As the field begins to open up, U.S. surgeons who opt to consider SMILE for their practices may be interested in the perspective of early adopters.
Advantages over predecessors. Overall, “SMILE has advantages over LASIK in that there is no flap—and advantages over PRK in terms of quicker recovery time,” said Jason E. Stahl, MD, who practices in Overland Park, Kansas.
In addition to doing away with the risk for traumatic flap displacement, SMILE is thought to offer better biomechanical corneal stability than LASIK and appears to place patients at lower risk for postoperative dry eye symptoms. From a workflow standpoint, patients don’t need to be moved from 1 laser platform to another.3
SMILE also offers advantages over its immediate predecessor, FLEx (femtosecond lenticule extraction), said John F. Doane, MD, who practices in Kansas and Missouri. “Instead of a small incision, the FLEx procedure requires a large incision, creating a LASIK-type flap that has to be lifted and peeled back to reach the lenticule—and then repositioned after the lenticule is removed,” said Dr. Doane. The result: a longer recovery time than that experienced by SMILE patients.
Visual outcomes. Clinical safety and effectiveness data for SMILE submitted to the FDA demonstrated stable vision correction at 6 months, with all but 1 of the 328 participants experiencing uncorrected visual acuity (VA) of 20/40 or better, and 88% experiencing uncorrected VA of 20/20 or better.4
Patients enrolled in this study had spherical myopia in the range of –1 D to –10 D and up to –0.50 D cylinder. SMILE was performed in 1 eye, and the nonstudy eye was treated with LASIK outside the clinical study.
Postoperative complications. In a study of more than 1,500 SMILE procedures, postoperative complications included trace haze (8%), epithelial dryness on postop day 1 (5%), interface inflammation secondary to central abrasion (0.3%), and minor interface infiltrates (0.3%).5 Only 1 patient experienced corrected distance VA (CDVA) difficulties at 3 months.
Long-term results. Given SMILE’s status as a relative newcomer, long-term results are somewhat limited. But in a study of patients with high myopia (45 eyes of 35 patients with mean spherical equivalent of –7.10 ± 0.95 D), 86% of eyes with plano target had an uncorrected distance VA of 20/20 or better at 2 years after SMILE. All told, 2% of eyes lost 1 line of CDVA, while 32% gained 1 line.6
And 5-year results of the first cohort of international patients to undergo the procedure found that initial outcomes proved stable, and no late complications were observed.7 CDVA improved from 0.02 (in logMAR) at 1 month postoperatively to –0.12 at 5 years, and 32 of the 56 eyes evaluated (58%) experienced a gain of 1 or 2 lines in vision. All patients were routinely treated for dry eye symptoms within the first 3 months postoperatively; after this point, none of them needed further dry eye treatment.
A Procedural Primer
The FS laser delivers about 17 million spots in the cornea in 34 seconds, creating what has been compared to a perforated piece of paper, said Dr. Doane. The benefit of these perforations in SMILE is that they allow the lenticule to be easily removed.
To begin SMILE, the patient is raised to the contact glass of the FS laser, followed by activation of the suction ports to keep the patient’s eye fixated in the correct position while the instrastromal lenticule is created.
Surgical steps. Dr. Doane provided a basic outline of the 4 surgical steps involved.
Posterior photodisruption. This uses an out-to-in direction of the laser. It determines the refractive power change (horizontal plane) of the lenticule, which can range from 6 to 7 mm.
Lenticular side cuts. In this step, incisions are made around the perimeter of the lenticule (vertical plane).
Anterior photodisruption (cap cut). This uses an in-to-out direction of the laser (horizontal plane). It takes place parallel to the corneal surface; for the United States, it is set at 120 μm.
A single incision side cut. This occurs at the superior position, with a width of 2.5 to 4.0 mm (vertical plane), to access the pocket to remove the lenticule.
Patient repositioning. The patient is then repositioned to the surgical microscope portion of the FS laser for the separation and extraction of the lenticule.
|
Challenges and Pearls
Refractive surgeons who are considering introducing SMILE into their refractive practice—described as “the leap from flap to cap”—have several challenges to consider.
Learning curve. The initial learning curve can be steep, a fact that Dr. Doane attributes to the 3-dimensional nature of the procedure.
“For example, in LASIK, you peel back a flap and have direct visualization when ablating the corneal tissue with the excimer laser,” he said. In contrast, “SMILE requires surgeons to see in 3-dimensional space, and it can get confusing if you don’t have the experience. You have to trust [that] the laser has done what you programmed it to do. After 5 to 10 cases, you start feeling comfortable.” Dr. Stahl agreed. “It is a new technique—freeing the lenticule and then extracting it.”
One practice’s experience. Dr. Stahl and his colleagues purchased the VisuMax laser in December 2016, 3 months after FDA approval. They spent the next 3 months becoming comfortable with the laser.
Initially, they made flaps to “understand the device’s unique features,” Dr. Stahl said. They also took wet lab courses to learn the procedure and viewed videos from experienced surgeons. Their first day of SMILE surgery occurred in March 2017, and their hands-on learning curve went smoothly, as the procedure became “quite easy” after a few cases, he said.
Patient selection. “Patients who are LASIK candidates are also SMILE candidates, and from a biomechanical standpoint, SMILE appears stronger. We are interrupting fewer corneal nerve fibers, which in turn may minimize dry eye,” said Dr. Doane. He added, “I have patients who had SMILE in 1 eye and LASIK in the other, and their vision on postop day 1 was identical.”
“SMILE is not suitable for patients who are extremely anxious about undergoing refractive surgery or exhibit difficulty keeping their eyes open,” Dr. Dishler said, as this can contribute to loss of suction (see below). And as with LASIK, patients with keratoconus are not good candidates for SMILE.
Potential surgical complications. These include anterior cap and side cut tears, difficult lenticule dissection, and retained lenticule fragments.8
Potential loss of suction. The FS laser uses very low suction pressure to hold the eye, Dr. Stahl said. “If the patient moves or squeezes [the eyelids to blink], you can lose suction more easily than with other FS lasers. If you lose suction, you may need to convert to LASIK or PRK.” To minimize this risk, he suggested providing “verbal anesthesia,” talking the patient through the procedure with a calm, reassuring voice as the laser cuts the lenticule.
Incomplete lenticule removal. This potential complication is unique to SMILE, Dr. Stahl noted. He added that it is imperative for the surgeon to thoroughly inspect the lenticule upon completion of the dissection and removal—and that “if the surgeon finds that the lenticule is not complete, he or she must find the residual piece of lenticule and remove it.”
Need for touch-ups. Enhancements may be needed in cases of under- or overcorrection as well as in those of irregular astigmatism occurring as a result of decentered treatment, difficult lenticule dissection, or partially retained lenticule fragments.
Rates and risks. A study conducted in Singapore and published last year found that the incidence of enhancement after SMILE was 2.1% and 2.9% at 1 and 2 years, respectively.8 Patients with greater initial refractive error (preoperative myopia > 6 D and preoperative astigmatism > 3 D) had higher enhancement rates. Intraoperative suction loss also was found to be a contributing factor.
At present, if an enhancement is necessary, PRK is recommended, Dr. Stahl said. However, if future software approvals increase the current laser parameters, this may allow LASIK enhancements to be performed after SMILE in certain eyes.
Patient Feedback
With regard to patient acceptance, “I offer both LASIK and SMILE to qualifying spherical myopia candidates. What I have found is that patients are excited about fast visual recovery, less dryness, and no flap,” Dr. Stahl said. He cited the admittedly unusual example of a patient who is a professional wrestler. The man chose SMILE because he did not want to worry about a flap being dislodged in the ring.
And Dr. Dishler reported that SMILE resonates with his active, millennial patients who want to return to their normal activities without a lot of “fussing” over their postoperative care. “The reality is that, beyond [my need to] see them 1 day postop and check them a month later, they tend to do well and do not need any subsequent appointments, although they are seen at 6 and 12 months postop for completeness.”
___________________________
1 www.carlzeiss.com.
2 Marino G et al. Asia-Pac J Ophthalmol. 2017;6(5):456-464.
3 Ji YW et al. Am J Ophthalmol. 2017;179:159-170.
4 FDA approves VisuMax Femtosecond Laser to surgically treat nearsightedness. Silver Spring, Md.: U.S. Food and Drug Administration; Sept. 13, 2016. Accessed Feb. 22, 2018.
5 Ivarsen A et al. Ophthalmology. 2014;121(4):822-828.
6 Yıldırım Y et al. Turk J Ophthalmol. 2016;46(5):200-204.
7 Blum M et al. Br J Ophthalmol. 2016;100:1192-1195.
8 Liu YC et al. Ophthalmology. 2017;124(6);813-821.
___________________________
Dr. Dishler is in practice with the Dishler Laser Institute in Englewood and Aurora, Colo. Relevant financial disclosures: Carl Zeiss Meditec: C.
Dr. Doane is in practice with Discover Vision in Leawood, Kansas, and Independence, Mo. Relevant financial disclosures: Carl Zeiss Meditec: C.
Dr. Stahl is in practice with Durrie Vision in Overland Park, Kansas. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Dishler Carl Zeiss Meditec: C.
Dr. Doane Carl Zeiss Meditec: C; Presbyopia Therapies: O; RxSight: C.
Dr. Stahl None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|