Download PDF
Despite lingering questions about the causes of a burgeoning myopia epidemic, a network meta-analysis of 30 randomized controlled trials (RCTs) involving 5,422 eyes has found that more than one effective intervention exists for slowing myopia progression in children.1 “We have clear evidence that the gold standard—simply treating children with glasses—falls far short by comparison,” said coauthor Ian Flitcroft, DPhil, FRCOphth, ophthalmologist at the Children’s University Hospital in Dublin, Ireland.
The study looked at 16 interventions with a treatment duration of at least 1 year. The primary outcomes were mean annual change in refraction and mean annual change in axial length—a quicker, more accurate method than refraction for assessing myopia, he said.
 |
SOLUTIONS IN SIGHT? Childhood myopia is a growing problem. A recent meta-analysis compared 16 methods theorized to slow its progression.
|
Effective therapies. Consistent with previous results, pharmacologic treatments were found most effective. Although high-dose atropine (1%) showed the strongest benefit among all therapies in curbing myopia progression, low-dose atropine (0.01%) was almost as effective—and had minimal side effects. “That’s the real game-changer,” said Dr. Flitcroft. “However, the big caveat here is that almost all the atropine studies came from 1 racial group: Asians.”
In addition, 3 other approaches—orthokeratology, soft contact lenses with peripheral defocus–modifying designs, and progressive addition spectacle lenses—significantly slowed myopia progression in terms of refraction or axial length. Other interventions studied had minimal or statistically insignificant effects.
The researchers also found that Asian children appeared to benefit more from treatment than white children and that most interventions were less effective during the second year of treatment.
Robust information. In the past, most studies of myopia interventions lacked multiple head-to-head comparisons. Unlike a conventional pairwise meta-analysis, this network meta-analysis simultaneously analyzed both direct and indirect comparisons of interventions based on a common comparator, providing increased sample size and more robust information.
“It allowed us to create a single theoretical trial, ranking and comparing multiple interventions in a consistent way,” said Dr. Flitcroft. In addition, the researchers performed sensitivity analysis to ensure that trials with unusually good or bad results did not skew the average and change the conclusions.
Time to act? This trial is just the beginning, not the end of the story, said Dr. Flitcroft. Myopia control is an entirely new therapeutic area, he said, with no protocols or guidelines; and many questions remain about whom to treat and when, as well as long-term safety and tolerability.
However, Dr. Flitcroft challenged colleagues to consider acting sooner rather than later. “High levels of myopia lead to myopic maculopathy, one of the top 5 causes of blindness in the working-age population in the United States and other countries,” he said. “And even low levels of myopia increase the risk for macular degeneration, glaucoma, cataract, and retinal detachments.”
This meta-analysis now shows what’s effective, he said, adding, “How effective does a treatment need to be before we use it?”
—Annie Stuart
___________________________
1 Huang J et al. Ophthalmology. 2016;123(4):697-708.
___________________________
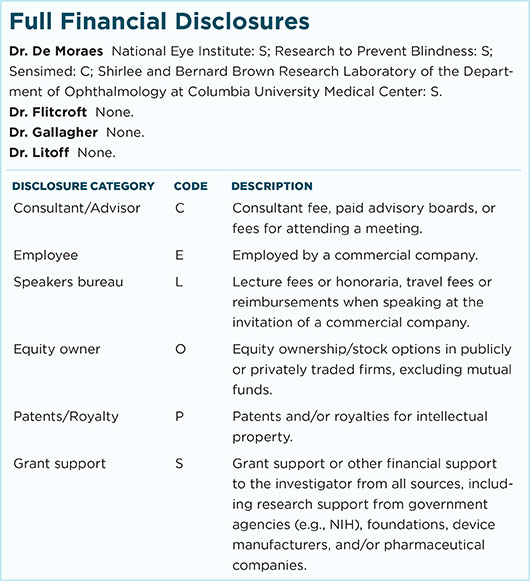
Relevant financial disclosures: Dr. Flitcroft—None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review