By Katherine J. Williams, MD, and Richard C. Allen, MD, PhD
Edited By: Ahmad A. Aref, MD, MBA
Download PDF
The parents of Macie Caldwell,* a 4-year-old girl, were becoming increasingly worried. For the past year, Macie had redness in the corner of her eye. What’s more, over the last few months, the lesion was growing.
The Presentation
Macie’s parents said that their daughter was a healthy and happy child, and they hadn’t noticed any recent changes in her behavior. She had met her developmental milestones, was on no medications, and had not experienced any trauma. She had been seen for cervical lymphadenopathy about a year previously, but otherwise had no medical problems. Her parents stated that they hadn’t noticed any tearing or photophobia. There was no family history of ocular problems.
On evaluation at an outside clinic, Macie’s vision was 20/25 in each eye; her intraocular pressure was normal to palpation; and her pupils were equal and reactive in each eye without afferent pupillary defects. Visual fields were full in both eyes, as was motility.
The external exam revealed a right medial canthal lesion with a fleshy appearance, and it was slightly difficult for Macie to close that lid, resulting in mild nasal lagophthalmos. The external exam was normal on her left side.
The anterior segment exam was normal bilaterally, as was the fundus examination.
Because the lesion was growing in size, and there was mild lagophthalmos, Macie was referred to ocular oncology for further evaluation.
We Get a Look
In the ocular oncology clinic, we noted that Macie had a nontender lesion that appeared to extend from the caruncle (Fig. 1).
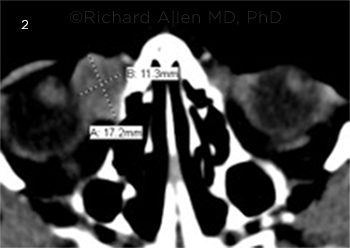
After examining Macie, we recommended that she undergo additional imaging with computed tomography (CT) of the orbits with contrast. The CT scan (Fig. 2) revealed a heterogeneously rim enhancing mass measuring 1.7 cm × 1.7 cm × 1.3 cm. This lesion was medially proximal to the inferomedial aspect of the globe; it was also proximal to the insertion of the medial rectus without involvement of the inferior rectus muscle. We decided to examine Macie under anesthesia, and an excisional biopsy of the lesion was performed by the oculoplastic surgery service.
 |
|
WE GET A LOOK. Medial canthal lesion of right eye with fleshy appearance.
|
What the Pathology Showed
Histopathology revealed a well circumscribed lesion with medium to large cells, which were stained with CD68 (used for macrophages and other monocytes), S100 (used for peripheral nerve sheath tumors), and CD1a (used for Langerhans cells). Histiocytes showed emperipolesis (the presence of an intact cell within the cytoplasm of another cell). Immunostaining was negative for Melan-A and glial fibrillary acidic protein (GFAP).
Of note, the percentage of IgG4 was calculated in each of three fields under microscopic evaluation, and it ranged from 6% to 28%. As none of the fields was greater than 40%, this result was not considered to be indicative of IgG4 disease but was noted to be elevated.
The overall features were suggestive of extranodal sinus histiocytosis with massive lymphadenopathy—i.e., Rosai-Dorfman disease.
 |
|
IMAGING. Noncontrast CT of orbits shows a heterogeneously rim enhancing mass, medial to the inferomedial aspect of the globe and proximal to the insertion of the medial rectus.
|
Management
We referred Macie to hematology/oncology for further management.
The hematology service confirmed that no rash, bone pain, or mouth sores were evident but did note that a prior CT of the soft tissues of the neck with contrast from a year before the biopsy showed a nodular enhancing lesion in the parotid gland; at that time, this finding was thought to be not concerning and consistent with reactive lymphadenopathy. On exam, bilateral cervical lymphadenopathy was noted with nodes measuring 4.5 cm × 3 cm with firm indiscrete borders. A whole-body positron emission tomography (PET) scan confirmed that there was intensely hypermetabolic bilateral cervical adenopathy consistent with Rosai-Dorfman disease. No additional extranodal or nodal disease below the neck was observed.
After this confirmation with PET CT, Macie underwent venous access port placement and started therapy with intravenous clofarabine.
Discussion
First described in 1969 and 1972 by Juan Rosai and Ronald Dorfman, respectively, as a benign sinus histiocytosis with massive lymphadenopathy, Rosai-Dorfman disease is a rare disorder with mean age of onset between 13 and 20 years of age.1,2
Etiology. Although the etiology of Rosai-Dorfman is unknown, viral and bacterial etiologies have been implicated, including Epstein-Barr virus, parvovirus B19, and Klebsiella.3,4
Presentation. Although patients may present with fevers and leukocytosis, painless lymphadenopathy is the most frequent presenting sign of Rosai-Dorfman.2,3
The disease is clinically characterized by extranodal manifestations in the eye, upper respiratory tract, salivary glands, skin, bone, meninges, central nervous system, and testis.
In the orbit, Rosai-Dorfman typically appears unilaterally; bilateral orbital masses are very rare, and only a few cases have been described to date with bilateral involvement.5 Additional ocular presentations include uveitis or serous retinal detachments. Involvement in the uveal tract is thought to be related to expression of a proliferative process and is suggestive of a pseudo-uveitis.6,7
Histopathology. Review of the excised lesion with histopathology is crucial in the diagnosis of Rosai-Dorfman disease. Characteristics include proliferation of foamy histiocytes with round nuclei, pale cytoplasm, and staining with S100 immunophenotype protein.2,6 The cells also showed emperipolesis. This is an uncommon process in which the engulfed cell is not killed by the lysosomal enzymes of the macrophage but rather exists as a viable cell, which can exit at any time without structural damage to either cell. Emperipolesis is seen in tumor giant cells in Hodgkin disease as well.8
In a case study, Rosai-Dorfman has been reported as having S100 positive non-Langerhans histiocytes with emperipolesis with plasma cells positive for IgG4 in the orbit in a 9-year-old Black boy.9 Varying levels of IgG4/IgG ratios have been previously observed in other regions of lymphadenopathy, including axillary and cervical lymph nodes. In a study of 70 patients with Rosai-Dorfman disease, 12 patients had >40% IgG4/IgG positive cells; of these, there was a preponderance of males (nine males and three females) and the median age was 55 years, which was significantly higher than the median age (27 years) of the IgG4/IgG <40% patients.10
Rule out malignant diagnoses. Rosai-Dorfman is a benign disorder of non-Langerhans cell histiocytosis, and it is important to differentiate it from malignant causes of lymph node enlargement and lymphocytic proliferation.11 The natural course of Rosai-Dorfman is typically self-limiting with spontaneous regression. However, life- or function-threatening conditions may require further surgical or medical therapy.12
Management. Primary management of the ophthalmic manifestations can consist of surgical excision,3 though observation may be reasonable depending on the size and location of the lesion. Recurrence may occur, and observation can be considered for mild manifestations. If debulking is needed, systemic corticosteroids, chemotherapy, and radiotherapy have all been suggested. For orbital involvement, treatment goals include controlling aspects that threaten function, and chemotherapy has been utilized in cases of visually threatening optic nerve compression.13,14
Age of our patient was unusual. Our case is particularly interesting given the young age of the patient at presentation, as well as the trend toward slightly higher IgG4 involvement than expected based on age and gender. Ophthalmologists should be careful to include malignant lymphocytic proliferative disorders in the differential of Rosai-Dorfman disease. Close consultation with the pathologist regarding the history of the lesion may help in securing the correct interpretation and diagnosis.
___________________________
*Patient name is fictitious.
___________________________
1 Foucar E et al. Am J Ophthalmol. 1979;87(3):354-367.
2 Foucar E et al. Semin Diagn Pathol. 1990;7(1):19-73.
3 Vemuganti GK et al. J Hematol Oncol. 2008;1:7.
4 Harley EH. J Natl Med Assoc. 1991;83(10):922-924.
5 Narjess BR et al. Can J Ophthalmol. 2019;54(2):e77-e81.
6 Meyer CH et al. Arch Ophthalmol. 2003;12(5):733-735.
7 Tan HY, Kao LY. Chang Gung Med J. 2002;25(9):621-625.
8 Rastogi V et al. J Clin Diagn Res. 2014;8(12):ZM01-ZM02.
9 Mudhar HS, Duke R. Orbit. 2013;32(5):315-317.
10 Menon MP et al. Histopathology. 2014;64(3):455-459.
11 Khan AA et al. Hematol Oncol Stem Cell Ther. 2011;4(2):94-96.
12 Komp DM. Semin Diagn Pathol. 1990;7(1):83-86.
13 Pulsoni A et al. Am J Hematol. 2002;69(1):67-71.
14 Lee-Wing M et al. Am J Ophthalmol. 2001;131(5):677-678.
___________________________
Dr. Williams is an ASOPRS oculoplastics fellow at Baylor College of Medicine. Dr. Allen is a professor of ophthalmology and oculoplastic surgery at Baylor College of Medicine and MD Anderson Cancer Center in Houston. Financial disclosures: None.