By Archana Nair, MD, MS, Akash Gupta, MD, Payal Patel, MD, and Irina Belinsky, MD
Edited By: Steven J. Gedde, MD
Download PDF
Johnathan Goldstein* was a healthy 4-year-old boy. One Friday morning, his mother noticed that his left eyelid was red and swollen. When the swelling worsened the following morning, she took him to their local urgent care facility. She was given erythromycin ointment to apply at home, but by the evening the swelling dramatically worsened. Noting that her son had now also developed pain and restricted upward gaze in the left eye, she drove him to the emergency room for further evaluation.
We Get a Look
Presentation. When Johnathan’s history was taken in the ER, his mother said that he hadn’t had any fevers, chills, change in appetite, upper respiratory symptoms, or trauma.
On exam, he appeared well, he was afebrile, and his vital signs were normal. The ocular examination disclosed a visual acuity of 20/20 in each eye, equally round and reactive pupils with no afferent pupillary defect, and eyes soft to palpation bilaterally. There was partial restriction of the left eye in upward gaze and the globe was slightly displaced inferiorly, but motility was otherwise normal.
His left upper eyelid was markedly swollen and red; the overlying eyelid skin was intact without fluctuance (Fig. 1). There was no discharge from the eye or surrounding tissue. The rest of the anterior and dilated exam were normal.
Our first impressions. At this point, there was concern for preseptal or orbital cellulitis. Given Johnathan’s young age and clinical presentation, he was admitted to the hospital and started on IV ampicillin-sulbactam. After three days, there was no improvement. He now had more upgaze restriction and developed new chemosis superiorly (Fig. 2). The infectious disease team added IV vancomycin.
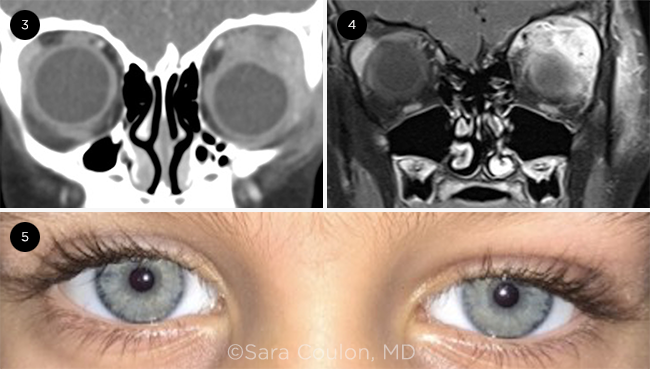
Imaging. We ordered contrast computed tomography (CT) of the orbits. It showed pre- and postseptal and extra- and intraconal soft tissue enhancement, and an enlarged left lacrimal gland (Fig. 3). Paranasal sinuses were clear. A low density area in the intraconal space raised the possibility of an abscess, so we ordered follow-up magnetic resonance imaging (MRI). There was in fact no abscess, but there was redemonstration of an enlarged lacrimal gland, and the MRI highlighted associated enlargement and enhancement of the superior and lateral recti muscles with scleral thickening of the posterolateral aspect of the globe (Fig. 4).
Labs. Bloodwork continued to show a normal white blood cell count and a normal C-reactive protein. Syphilis and tuberculosis testing were negative. The erythrocyte sedimentation rate (ESR) was mildly elevated. Infectious disease history was negative for travel or exposure to cats.
 |
|
WE GET A LOOK. The patient’s left eye (1) when he first presented at the ER and (2) three days later, with increased superior chemosis and restriction of upgaze.
|
Switching Gears
At this point, our concern shifted from orbital cellulitis to dacryoadenitis, either infectious or inflammatory. Lacrimal gland malignancy was low on the differential because he was a healthy boy with a normal physical exam and no radiographic characteristics of tumor.
Rheumatologic workup for angiotensin-converting enzyme (ACE), rheumatoid factor (RF), uric acid, antineutrophil cytoplasmic antibodies (ANCA), and antinuclear antibody (ANA) were all negative.
Given that Johnathan had not shown any improvement on IV antibiotics, had a reassuring MRI without abscess, and had no systemic signs of infection, we started him on IV steroids (1 mg/kg) for presumed idiopathic orbital inflammation (IOI).
Making the Diagnosis
In a typical case of IOI, we would expect treatment with high-dose steroids to result in rapid improvement within two or three days. However, five days after adding steroids, Johnathan’s extraocular motility and edema were only minimally improved.
Given the ongoing diagnostic dilemma, a biopsy of the lacrimal gland was taken. Intraoperatively, we noted that the gland was enlarged and hardened, with effacement of its normal architecture. The surrounding tissues—including orbital fat, periosteum, and bone—were normal. Histopathologic examination showed “idiopathic inflammation”: infiltration of the lacrimal gland by a mixed population of inflammatory cells consisting primarily of mature lymphocytes, as well as eosinophils, plasma cells, and neutrophils, without other histologic abnormality. There was no granulomatous inflammation.
Johnathan was discharged from the hospital on a slow oral steroid taper. Within two weeks, his exam was markedly improved (Fig. 5). Outpatient testing by his pediatrician for Epstein-Barr virus immunoglobulin (Ig) M was positive, and IgG was negative, establishing the diagnosis of infectious mononucleosis (IM)–related dacryoadenitis. He was continued on steroids and followed up in our clinic with resolution of his symptoms over the next month.
 |
|
TREATMENT. After reviewing the (3) CT and (4) MRI, we started Johnathan on steroid treatment; (5) left eye two weeks after discharge from hospital.
|
Discussion
The cause of acute dacryoadenitis is most commonly viral infection or noninfectious inflammatory disease, such as sarcoidosis or idiopathic orbital inflammation.1 Infectious dacryoadenitis is believed to be caused by hematogenous spread or direct inoculation from the conjunctiva through the lacrimal ducts into the lacrimal gland.2 About 50% of infectious cases are bilateral.2
In children, the most common cause are viruses, such as mumps, measles, influenza, scarlet fever, or erysipelas.3 Dacryoadenitis has also been documented in the setting of tuberculosis in isolated case reports.4 Adult infectious dacryoadenitis is associated with diabetes and immune-deficient states.3
Chronic dacryoadenitis is suggestive of autoimmune disorders such as Sjögren syndrome, thyroid disease, IgG4-related disease, or vasculitis. Malignancy must also be considered in the differential, particularly in adult patients unresponsive to treatment, and a biopsy may be necessary to rule out this diagnosis.5
Infectious mononucleosis. Dacryoadenitis is a rarely reported manifestation of IM. However, IM has an affinity for lymphoid tissues, and it has been postulated that upper eyelid edema, often seen with these patients, may be caused by subtle lacrimal gland involvement of the viral infection.6 IM can cause a wide variety of ocular symptoms, often without other systemic signs of IM. Ocular features of IM associated with Epstein-Barr virus include dacryocystitis, conjunctivitis, episcleritis, keratitis, uveitis, optic neuritis, retinitis, ophthalmoplegia, and facial nerve palsy.7
A rare condition. Reports in the literature of clinically significant dacryoadenitis—especially, as in this case, with an identified viral cause—are rare. In children with dacryoadenitis, infectious mononucleosis should be included in the differential. However, this diagnosis requires a high index of suspicion. Given the rarity of this presentation, it’s advisable to include Epstein-Barr virus immunoglobulin in the workup to help in early identification of the disease and help guide early treatment for these children.
___________________________
* Patient name is fictitious.
___________________________
1 Rootman J. Diseases of the Orbit: A Multidisciplinary Approach. 2nd ed. Lippincott Williams & Wilkins; 2003.
2 Fay A, Dolman PJ. Diseases and Disorders of the Orbit and Ocular Adnexa. 1st ed. Elsevier; 2016.
3 Lacrimal Gland Tumor Study Group. Jpn J Ophthalmol. 2005;49(5):343-348.
4 Ruman-Colombier M et al. Pediatr Infect Dis J. 2017;36(1):117-119.
5 Bowling B, Kanski JJ. Kanski’s Clinical Ophthalmology: A Systematic Approach. 8th ed. Elsevier; 2016.
6 Aburn NS, Sullivan TJ. Ophthalmology. 1996;103(5):776-778.
7 Matoba AY. Surv Ophthalmol. 1990;35(2):145-150.
___________________________
Dr. Nair is a second-year ophthalmology resident; Dr. Patel is a specialist in oculoplastics and is a clinical assistant professor; Dr. Belinsky is a specialist in oculoplastics and ocular oncology, and is a clinical assistant professor; all three are at New York University Langone Health in New York City. Dr. Gupta is a postdoctoral research associate at Yale School of Medicine in New Haven, Conn. Relevant financial disclosures: None.