By Scott E. Laborwit, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
In recent years, many ophthalmologists have begun integrating femtosecond laser–assisted cataract surgery (LACS) into their practice. Most cataract surgeons are very comfortable with their current technique, and introducing LACS is a major shift away from this comfort zone. Learning any new technique may cause some anxiety; in the case of LACS, this may be increased because patients who are paying out of pocket for a procedure often have higher expectations for the outcome and lower tolerance for complications.
This article offers practical tips, based on my experience with more than 4,000 cases, to assist ophthalmologists who are beginning to incorporate this new technology into their surgical approach.
The Basics: Training, Logging, Patient Protocol
Comprehensive training should be the first priority, not only for performing the surgical techniques but also for operating the equipment itself. It is important to pay attention to the device and process details as both a surgeon and a laser technician. Become familiar with aspects of the device such as how data are entered, how to measure laser energy levels, and how to clear an error message—and develop a system to log this information. This log should have each surgeon’s settings recorded and dated as a reference.
Next, develop a plan that you and your team can follow immediately prior to each laser treatment. In our surgical center, each patient is counseled before entering the laser room on what to expect and how long each step will take. We also use a time-out to confirm the patient’s astigmatism treatment plan before each laser procedure.
 |
|
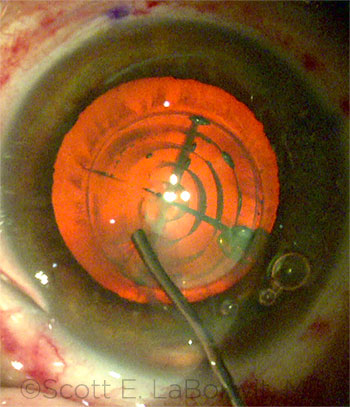
CHECKING CAPSULOTOMY. The viscoelastic cannula can be used to place downward pressure on the capsule to identify areas that are not free. Striae demonstrate an area of adherence; careful additional downward pressure will tear the bridging adhesion easily and complete the capsulorrhexis without need for a forceps.
|
Docking: Firm Headrest, Chin up, Wide Eyes
Surgeons who use a femtosecond laser to create a flap for LASIK surgery are already familiar with docking the patient interface (PI) to the eye. In fact, they typically find docking for cataract surgery easier, since the suction doesn’t raise the IOP quite as high.1
Head position. Positioning the patient’s head properly is the most important factor for optimal docking. The patient’s head should be on a firm surface to keep it from moving back during treatment, so remove any pillows or “donuts” and rest the patient’s head directly on the bed.
Make sure the chin is higher than the forehead to keep the upper lid out of the way. If the patient has a large nose, turn the head away from the PI so the nose doesn’t interfere with contact between the PI and the eye.
A strong wire lid speculum can be used to create a wide aperture. When you are docking, lower the PI until a layer of contact is about halfway across the cornea, and then apply suction. Too much contact can cause a trapped air bubble and limit laser treatment to that area of the eye.
Fixation. Patients will often look at the fixation light to center the eye. If they have trouble tracking, ask them to open their other eye and look straight ahead. Opening both eyes can also facilitate PI-to-cornea contact because it stops patients from squinting.
Extra lubricating drops can be helpful for difficult cases, such as patients with corneas that are very flat or steep.
Capsulotomy Considerations
With experience, each surgeon will develop a personalized approach to LACS. I have found the following pointers helpful in my practice.
Size and placement. Surgeons can specify the size and position of the capsulotomy. I prefer a 5-mm capsulotomy size to allow 0.5 mm of capsule to overlap the IOL, and I currently center this on the geometric center of the undilated pupil.
Recognize whether the capsule is free. Current LACS technology typically allows at least 97% of capsules to be free; indeed, some studies have found a rate of incomplete capsulotomies of less than 1%.2 For surgeons getting started with LACS, learning how to identify a capsular tag or a few clock-hours of uncut capsule is critical.
Trypan blue helps. While creating the capsulotomy, the laser cuts at least 250 μm into the cortex and 250 μm above the capsule into the anterior chamber. The cortex becomes cloudy when it is cut, making it more difficult to see the capsule clearly and giving a pseudo-cut appearance. Consider using Trypan blue, at least for your first few cases, to help distinguish between capsule and cortex and ensure that the capsular button is free.
Use viscoelastic. Inspect for any suspicious areas before placing viscoelastic into the anterior chamber. To further investigate an area of suspected capsular adherence or tag, fill the chamber with viscoelastic, and then use the viscoelastic cannula to tap down on the capsule approximately 1 mm away from the cut toward the visual axis.
Look for striae. You’ll know there’s a tag if there are striae extending distal to the expected cut area; at this point, more downward pressure with the cannula will typically break the tag.
Convert if necessary. If the adherence is more than a tag, a Utrata forceps can be used to convert to a traditional capsulorrhexis. Tear the capsule while it is folded over on itself and make the opening wider than the one created by the laser.
Ensure that the capsular button is out of the eye. Once the capsule is free, watch it closely to avoid finding it in the angle the next day. To avoid pushing the button into the angle while injecting viscoelastic into the anterior chamber, place the cannula distal to the button, and then inject viscoelastic to keep the capsule in its native position while watching closely.
It is also best to grab or visualize the button as it leaves the eye to make sure that it is no longer in the anterior chamber, especially if you are using dispersive viscoelastic.
Freeing the Lens
Use gentle injection. When hydrodissecting, be sure to protect the posterior capsule by minimizing the volume of fluid. Otherwise, the lens may float up, and pressure behind the lens can allow a posterior air bubble to burst through, rupturing the posterior capsule.3
Consider viscodissection. I find it helpful to use a dispersive viscoelastic to viscodissect the anterior capsule to the equator a full 270 degrees, while sparing the subincisional quadrant. Doing so breaks up a significant number of adhesions between the anterior capsule and the lens, while air bubbles pneumodissect the posterior lens adhesions. With this technique I no longer need to rotate the lens during removal of the nucleus.
Nuclear Removal: Transition Slowly
Start with traditional methods. Surgeons who are adopting LACS may wish to use traditional techniques for nuclear removal during the transition. It is important to gain comfort and expertise by first integrating the previous steps in the procedure. Applying laser patterns to the lens will eventually aid in lens removal, but there is no need to climb this learning curve early on.
The precision of the laser, coupled with the benefit of imaging, offers surgeons opportunities for enhancing their cataract surgery technique. Applying these tips will help ease the transition as you begin to incorporate femtosecond laser into your cataract practice. Finally, remember that you can always revert to your traditional methods if a step becomes difficult.
___________________________
1 Schultz T et al. J Cataract Refract Surg. 2013;39(1):22-27.
2 Donaldson KE et al; ASCRS Refractive Cataract Surgery Subcommittee. J Cataract Refract Surg. 2013;39(11):1753-1763.
3 Yeoh R. [Letter]; Roberts TV et al. [Response]. J Cataract Refract Surg. 2012;38(4):730.
___________________________
Dr. LaBorwit is president of Select Eye Care in Towson, Md., and assistant professor of ophthalmology, part-time faculty, at the Wilmer Eye Institute. Relevant financial disclosures: Alcon: C.
See the disclosure key at www.aao.org/eyenet/disclosures.
Pearls for Astigmatic Keratotomy
Patients who have corneal astigmatism at the time of their cataract surgery may benefit from the use of femtosecond laser to perform astigmatic keratotomy (AK).
Obtain quality measurements. A laser-created AK incision is very precise because it is computer guided, using OCT images of the patient’s cornea. I treat the 9-mm optical zone with an 85% depth.
The results of AK will be only as good as the measurements and preparation. Creating a treatment plan for astigmatism management can be challenging when there is conflict between topographic, manual, and automated keratometry in the preop corneal astigmatism measurements.
First, evaluate the quality of each test. Second, initially perform manual keratometry personally, and over time, train only a few technicians to responsibly and reliably obtain this important piece of data. It is best to treat for the lower power of astigmatism to avoid flipping of the visual axis.
Mark the eye with the patient upright. Marking the eye with the patient sitting upright in the preop area prior to laser treatment will help line up AK incisions when the eye rotates while the patient is lying down.
The choice of marking device is based on personal preference. I have found the specialized marking devices to be cumbersome; and using a narrow vertical beam at the slit lamp was accurate, but time consuming. We now mark patients by hand with an ink pen; the person marking stands in front of the patient while the patient focuses on an object in the distance.
I prefer to mark superior at the 12 o’clock limbus; and instead of inferior, the eye is marked at the nasal limbus at 3 o’clock for the right eye and 9 o’clock for the left eye.
Make sure that the marks are placed firmly and at the limbus; faint marks will wash away with eyedrops, and if they are on the sclera they will be hard to see once the PI is docked. After PI docking, a cross pattern is overlapped on the image of the eye, which will allow you to rotate and easily line up these marks using the 90-degree angle.
Titrating the femto effect. A benefit of performing an AK with the femtosecond laser is that the effect can be titrated over time by extending the opening at the slit lamp 2 weeks later.
For example, when there are variable measurements of cylinder power, the laser can be set to create an AK for the higher power, but the surgeon can opt to open half or none of the AK at the time of surgery. If there is residual astigmatism 2 weeks later, a Sinskey hook can be used at the slit lamp to open the remaining AK.
Remember, you can always “unzip” the AK at a later time, but you can’t zip it back up.
|