When Techs See Patients: How to Get Paid Without Getting Into Trouble
By Sue Vicchrilli, COT, OCS, Academy Coding Executive
This article is from October 2007 and may contain outdated material.
Can a technician bill CPT code 99211 office or outpatient visit for the evaluation and management of an established patient and perform a visual field while the ophthalmologist is out of the office? Owing to regulations that say visual fields fall under general supervision, many ophthalmologists might answer yes.
But this is part of a larger issue: Under what circumstances can an assistant or technician bill an office visit? The answer lies in the Medicare Carrier Manual. An ophthalmologist can bill Medicare and be paid for health care that ophthalmic assistants and technicians provide. It’s called the “incident-to” benefit.
Incident-to requirements. To qualify as incident-to, the service must be:
- An integral part of an ophthalmologist’s diagnosis or treatment.
- Provided under the “direct supervision” of an ophthalmologist.
- Performed by an employee of that doctor.
- Something ordinarily done in a doctor’s office or clinic.
- Performed on a day when the doctor does not see the patient.
The doctor must have initial and ongoing involvement in the patient’s care. The ophthalmologist must see the patient first to diagnose the problem. The incident-to rules state that the “physician must perform the initial service for the patient and subsequent services frequently enough to reflect the doctor’s active participation in and management of the patient’s course of treatment.”
The doctor must provide “direct supervision.” In the office setting, this does not mean the doctor has to be in the same room. However, the physician must be present in the office suite and immediately available to provide assistance and direction throughout the time the ophthalmic medical personnel is performing services.
Provide adequate documentation. To warrant billing 99211, the documentation should include a written order detailing what components of the exam and testing services to perform. For example, the ophthalmologist might instruct the technician that in three months, when “Mrs. Snow” returns to the office, the technician should do the following: Record Mrs. Snow’s visual acuity; document the type of glaucoma medication and the time it was taken; and measure IOP and perform a specific visual field in both eyes. The above order needs to be documented in the medical record.
Warning: It can be easy to misuse 99211. Suppose the ophthalmic assistant or technician codes 99211 for taking K-readings and performing the A-scan before cataract surgery. The technician discusses the pre- and postop care with the patient. The physician does not see the patient on this date of service, so the staff member thinks that assigning the lowest E&M code, 99211, is a correct way to bill for the service. The error is that the A-scan and keratometry services are covered under the A-scan code (76519 or 92136) and the rest of the services are part of the global surgery package. Even though the visit takes place more than one day before the surgery, Medicare considers that the determination for surgery has already been made and therefore the preop paperwork and discussion performed by a nonpractitioner is part of the global package. To stress the message, the Correct Coding Initiative bundled CPT code 92136 IOLMaster with CPT code 99211 in April 2003. Then in July 2003, CPT code 76519 A-scan was bundled with the technician code as well.
 |
|
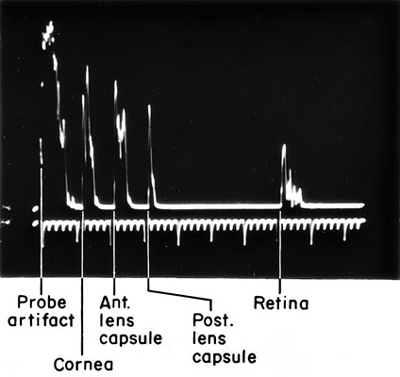
A-Scan. A common pitfall can occur when the tech performs an A-scan and then bills CPT code 99211.
|