By Raj K. Maturi, MD, and Lucius Walker
Edited by Thomas A. Oetting, MD
This article is from February 2009 and may contain outdated material.
It was Chloe Merton’s* young nephew who dialed 911. His father had sent him to drop off groceries for his Aunt Chloe, who was 35-weeks pregnant at the time. The boy hadn’t been at her house for long when, to his alarm, she slipped into unconsciousness for about 10 minutes. EMS soon arrived and rushed her to the nearby rural hospital.
When the 22-year-old woman was first admitted to the hospital, her blood pressure was 175/115. At her last prenatal visit, blood pressure had been normal, but—because she had missed a few visits—this was three months previously. It was noted that she already had a healthy 1-year-old child whose birth had been associated with preeclampsia. During that first pregnancy, her blood pressure was 190/140 at 38 weeks. Ms. Merton was otherwise healthy with normal blood pressures when not pregnant. Although she denied any recent drug use, she acknowledged that she was smoking two packs of cigarettes per day and had done so for eight years. In the obstetrics ward, signs of preeclampsia were noted—namely hypertension and proteinurea—as well as mild periorbital and facial swelling. She denied photophobia, blurry vision or other visual changes. A few hours after her admission, her blood pressure was 190/76 and she was placed on magnesium sulfate for induction. She refused spinal anesthetics and, under careful care of her obstetrician, gave vaginal delivery to a healthy 6-lb daughter. She required two units of blood postpartum due to loss during labor.
Ms. Merton doesn’t remember anything from the time of delivery, which was 10 a.m., until late in the afternoon when she recalls waking up and noticing severe loss of vision in both eyes.
The concerned obstetrician obtained a head CT, which showed no evidence of intracranial hemorrhage or cerebral edema. (The radiologist specifically examined the CT for petechial hemorrhages and focal edema in the occipital cortex.) This negative CT prompted an MRI scan, which was negative as well. The next day, her vision was no better.
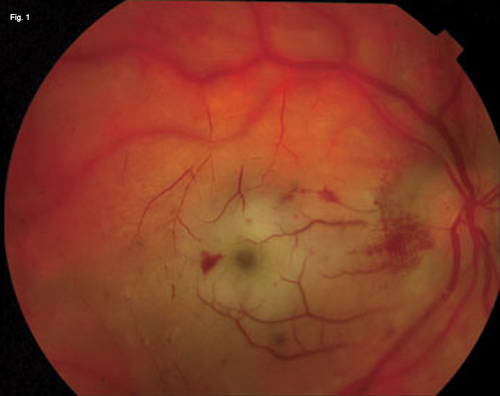
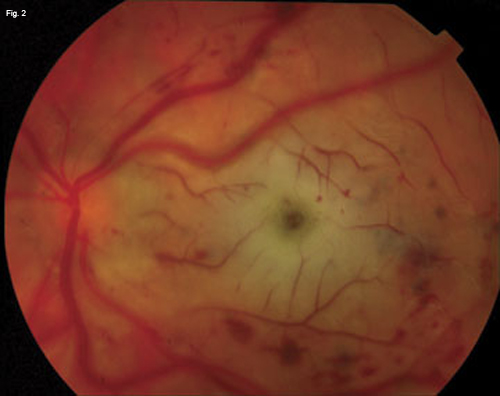
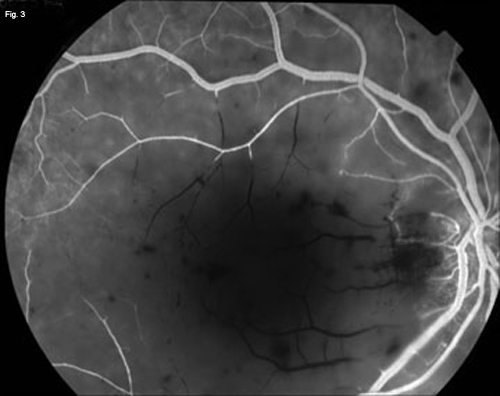
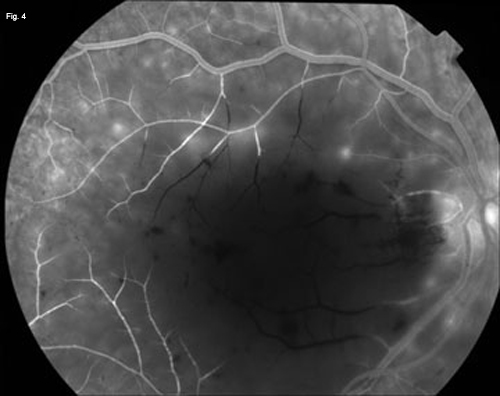
We get a look. We saw Ms. Merton a few days after she had given birth. Her vision had not improved. Visual acuity was light perception in each eye, with no afferent pupillary defect noted. The anterior segment exam was unremarkable, and the vitreous was free of inflammatory cells. Funduscopic exam demonstrated a “cherry red spot” centrally with massive macular edema and intraretinal hemorrhages bilaterally. Mild venous nicking was noted, and there appeared to be a closure of macular arterioles and venules (Fig. 1 and Fig. 2). The peripheral retina appeared relatively unaffected. A fluorescein angiogram revealed severe delay in perfusion of the macular vessels in each eye with late frames of the angiogram showing continued nonperfusion of the foveal vessels alone (Fig. 3 and Fig. 4).
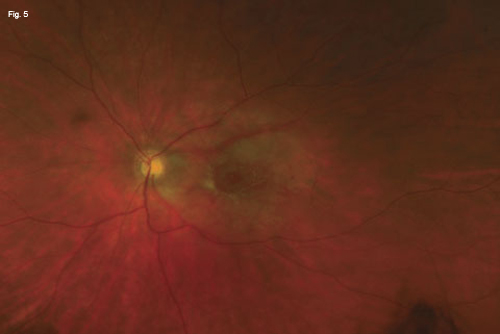
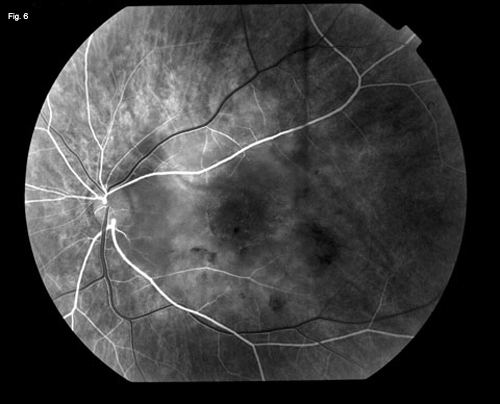
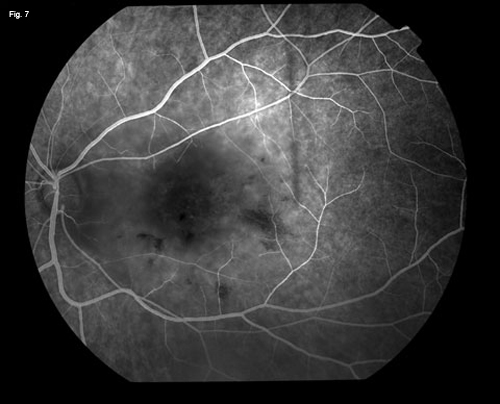
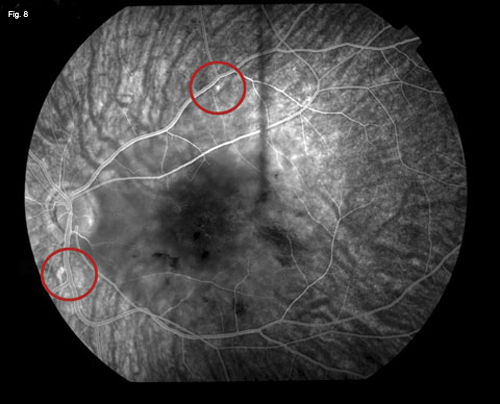
One month after delivery, her vision was count fingers in each eye, using eccentric fixation. Both maculae showed chronic changes from severe macular nonperfusion, including macular atrophy and areas of hyperpigmentation. We also noted Elschnig spots (Fig. 8).
Discussion. Preeclampsia is a rapidly progressive condition characterized by hypertension and proteinurea. It is estimated to occur in 5 to 8 percent of pregnancies. Visual disturbances occur in 25 to 50 percent of cases of preeclampsia and are characterized by photopsias, diplopia, scotomas and dimness of vision.1–3Pregnancy-induced hypertension can cause focal arteriolar spasms (this is noted in 10 to 40 percent of patients with preeclampsia), intraretinal hemorrhages and papilledema with exudate. Occasionally, more generalized arteriolar spasms can occur that result in temporary bilateral visual loss. Rare cases of permanent blindness have been reported due solely to arteriolar spasms.2 Serous retinal detachments that resolve spontaneously postpartum have been reported. Rarely, visual loss in preeclampsia also may occur in conjunction with amniotic fluid embolus or with thrombotic thrombocytopenic purpura. During pregnancy, coagulation disorders, such as disseminated intravascular coagulopathy (DIC), occur at a higher frequency in women with preeclampsia and can be associated with severe visual loss. A nonretinal etiology of postpartum severe bilateral visual loss includes cerebral edema in the occipital lobes.4 Visual function generally returns to baseline with resolution of cerebral edema. DIC is often caused by inflammatory cytokines that activate the coagulation pathway and result in severe thrombi in small vessels. DIC may also occur in the setting of amniotic fluid embolus.
Ms. Merton’s case. The severe small vessel thromboses seen in Ms. Merton’s retinal and choroidal circulation were consistent with DIC complicating a case of preeclampsia. While rare, such cases have been reported.5 A similar case of permanent visual loss was reported with a Purtscher-like retinopathy in the peripartum setting with hemolysis, elevated liver enzymes and low platelets.6
Over the next five months, Ms. Merton has noted a gradual increase in visual function. Two months after her visual loss, she was able to distinguish bright colors and, most recently, can read headlines in newspapers with her peripheral vision (20/200 in both eyes). She enrolled in a smoking cessation program and has accepted in-home low vision assistance, but refused psychiatric counseling for blindness.
___________________________
* Patient name is fictitious.
___________________________
1 Dinn, R. B. et al. Obstet Gynecol Surv 2003;58:137–144.
2 Lara-Torre, E. et al. Obstet Gynecol 2002;100:940–942.
3 Sunness, J. Surv Ophthalmol 1988;32:219–238.
4 Blodi, B. A. et al. Ophthalmology 1990;97:1654–1659.
5 Patel, N. et al. J Neuroophthalmol 2005;25:128–130.
6 Stewart, M. W. et al. Am J Ophthal 2007;143:886–887.
___________________________
Dr. Maturi is a vitreoretinal surgeon in private practice in Indianapolis and a volunteer clinical associate professor of ophthalmology at Indiana University. Mr. Walker is a third year undergraduate at Duke University. The authors would like to thank John Latona, MD, PhD, for his assistance.
|
|
|
We Get a Look. Both eyes (Figs. 1 and 2) demonstrate macular infarctions with massive retinal edema, a “cherry-red spot,” intraretinal dot-blot hemorrhages, occlusions of the perivascular small vessels, and generalized venous dilation. Early phase angiography of the right eye (Fig. 3) reveals complete nonperfusion of perifoveal small vessels. Late phase angiography (Fig. 4) demonstrates continued severe delayed filling of the foveal vessels, with diffuse staining of the perifoveal vessels.
|
|
|
|
One Month Later. Wide-angle photography of the left fundus (Fig. 5) reveals macular atrophy, disc pallor, some residual intraretinal hemorrhages and narrowed foveal vasculature. The peripheral retina is uninvolved. Early phase angiography (Fig. 6) reveals continued blockage of the macular arterioles and veins, with continued normal filling of peripheral retinal arterioles. Venous phase (Fig. 7) shows continued nonperfusion of the macular vessels. In the late frames (Fig. 8), a few Elschnig spots are seen with staining (red circles). There continues to be macular blockage due to the nonperfusion; the periphery appears essentially normal.
|