Download PDF
The COVID-19 pandemic was a defining event “that revealed the strengths and weaknesses of ophthalmic practices,” said Alan E. Kimura, MD, MPH. “It acted as a magnifier and an accelerant. It exposed both the opportunities and the threats that existed within every entity pre-COVID.”
How to survive and thrive. At Dr. Kimura’s practice—Colorado Retina Associates, in Denver—physicians and staff used the principles of lean practice management to adapt to the exigencies of the emergency. Below, several practice leaders explain how the lean approach helped them to navigate the crisis, and they describe the changes that they plan to keep in place beyond the pandemic. They are joined in their discussion by Aneesh Suneja, MBA, the consultant who helped initiate the lean transformation in each of their practices.
 |
|
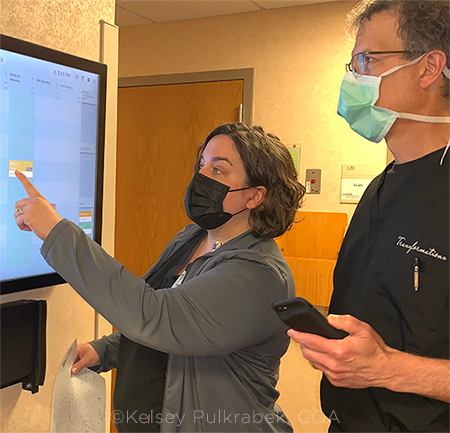
COVID PROMPTED A RETHINK ON SCHEDULING. In Dr. Lucarelli’s clinic, new scheduling procedures, remote scribing, in-room photography, and an electronic patient tracker were among the lean factors that reduced the average duration of patient visits by almost 40%. Above, Beth Pelar, COA, reviews the schedule with Dr. Lucarelli.
|
How Lean Helps in a Crisis
The lean approach provides a framework for experimenting with change: Staff members continually look for ways to improve processes, are empowered to make modifications, and gather metrics to see whether the revised procedures are a success, or if further changes are needed.
A team-based approach to iterative change. “We were able to transition and respond to the global health crisis due to our understanding of lean processes,” said Dr. Kimura. “Staff was already accustomed to altering our procedures expeditiously, sharing input, and working closely with our management team. We were therefore able to refine, as needed, the adjustments made during the days and weeks following the initial shutdown.”
Lean habits make it easier to respond to a crisis. Staff and physicians at Austin Retina Associates had a similar experience, said the practice’s CEO, Stephanie Collins Mangham, MBA, COA, OCSR, who emphasized their focus on metrics to evaluate the effectiveness of change. “Because our organization had been conducting [lean] trials for many years, and we were constantly looking for ways to improve, we were more agilely able to respond to the pandemic. Even though it was a stressful situation, we were ready,” she said.
Turning crisis into opportunity. “None of us will ever forget this pandemic,” said Mark Lucarelli, MD, FACS, an oculoplastic surgeon at University of Wisconsin (UW) Health in Madison. “The COVID-19 pandemic confronted us with unprecedented logistical challenges, but it also provided big opportunities for us to reexamine our processes and become more efficient.” Dr. Lucarelli is an oculoplastic surgeon who serves as the medical director of UW Health’s University Station Eye Clinic, where they began the implementation of lean principles in 2018.
What Is Lean?
The lean health care approach can be broken down as follows:
- Identify what it is that the patient values (e.g., reduced wait time).
- Review the processes that are used to provide those values and break each process down into its constituent steps. (This is known as value stream mapping.)
- Review each step to look for waste.
- Eliminate that waste.
How do you make a lean transformation? Lean is not a one-size-fits-all solution or a one-and-done endeavor. It is an ever-evolving process, as exemplified by Ms. Mangham’s practice, which continually tests ways to improve efficiency.
Use metrics to evaluate any changes. When Austin Retina tests a change in its processes, the evaluation will be based on metrics. Under the lean approach, tracking metrics is an integral part of perpetuating continued growth—after all, what can be measured, can be managed.
Gain a deeper understanding of your practice. In a lean transformation, a practice should study “every clinical task, remove waste, and optimize workflows,” according to Mr. Suneja. He emphasized that doing so “results in a deep understanding of clinical operations and enables both staff and leaders to quickly adjust to any emergency.”
Lean can work for any practice, no matter its size. The lean approach to practice management can be effective with any organization, no matter what size it is. “Whether you are managing a regional medical center or an academic medical center, or are operating as a solo practitioner, the fundamental premise of treating patients is immutable: It involves a team that focuses its efforts on caring for patients. Regardless of the various details, the fundamental challenges are the same, and the principles of lean can be effectively applied to efficiently improve your clinical processes and transform your practice,” said Dr. Lucarelli.
For more on lean, visit aao.org/lean.
|
You Need to Empower Staff, and They Need a Lean Champion
The lean approach will work only if it is a team effort.
Why you should empower your staff. “We were once a very top-down organization in that the administrators and physicians made all the decisions and then pushed them downstream to our staff,” said Ms. Mangham. “Now we are a very horizontal organization that empowers our employees. Through lean, we recognized that those on the front lines are the first to encounter problems and probably know better than most of us how to fix them. They have the clearest perspective of which process modifications will work and which will not.”
Build momentum: Success begets success. With lean, your staff “knows that their ideas for improvement are both valued and expected. They are your frontline change agents who should be constantly looking for ways to enhance clinic flow. Ultimately, the feeling of continual improvement snowballs and it can be a powerful experience for the entire organization,” said Dr. Lucarelli.
Don’t stall before you get started: Get out of the staff’s way! When organizations first try to adopt lean principles, one of the biggest obstacles to progress can be posed by leadership. “Some struggle mightily with relinquishing control and encouraging staff input,” said Dr. Kimura. “But they must get out of the way for the lean process to work.”
Who will champion the lean approach in your practice? At the heart of successful lean implementation is a clinic administrator and/or a physician—preferably both—who will lean into lean and fully embrace the philosophy. This should be “someone in a leadership role who is visionary and will buy into the ideology in such a way that it initiates a cultural shift in the organization,” said Ms. Mangham.
Reimagining Patient Flow
Social distancing prompted a reimagining of patient flow. When the pandemic struck, every clinic faced the challenge of keeping patients, staff, and physicians safe. As practices adopted a strategy of social distancing, they were forced to reengineer patient flow. This resulted in a “eureka” moment for some practices, as their new procedures resulted in significantly reduced patient wait times and increased satisfaction among both patients and staff. Under the lean approach, said Dr. Lucarelli, with its emphasis on minimizing waste and monitoring results, practices can set goals of maintaining and capitalizing on these improvements in efficiency post-pandemic.
Before the visit, prescreen patients. You can significantly reduce the amount of time patients spend at your clinic by gathering as much relevant information (such as their medical history and medication list) before they arrive at your office.
During the pandemic, Ms. Mangham decided to give prescreening a try at Austin Retina. It worked so well that the practice now has two full-time staff members devoted to the task. Working remotely, they call new patients to capture as much data as possible ahead of time. They also tell patients what to bring and what to expect during the visit. When the patients arrive at the clinic, a staff member will verify that nothing has changed since the prescreening.
Patients have been positive about being screened ahead of their visit. “Patients have been very receptive because they do not feel rushed to complete the required forms, and they appreciate knowing ahead of time what will occur during their visit,” said Ms. Mangham. “We will continue this practice post-COVID and are striving to take it further with our established patients in the future.”
During the visit, reduce the number of stops patients have to make. When Sanjay D. Goel, MD, opened his solo practice in January 2020, he could not have anticipated the quick impact COVID would have or the challenges it would present. With a firm understanding of lean, however, he was able to quickly reconfigure patient visits from seven stops in his clinic to three by cutting out unnecessary steps in the process. Patients now enter the office, receive a temperature check, and are taken to the technician lane for testing and, when necessary, dilation. Then the patient is taken to the exam lane and seen by Dr. Goel. “Prior to entering the room, I can look at all the scans and analyze the data on my iPad, so when I’m engaged, I perform a slit-lamp examination and discuss the options, making my time, and my patient’s time, in the clinic considerably more efficient,” he said.
Similarly, the UW Health’s oculoplastics service now conducts the majority of all pre- and post-op photography in the exam room, rather than having patients travel upstairs to another location in the clinic for this portion of the visit. “The old procedure was extremely wasteful and inefficient,” said Dr. Lucarelli. “Now the photos can be immediately uploaded into our electronic health record [EHR], where they can be reviewed, which saves our patients and care team a lot of time and steps.”
How the duration of a patient visit was cut by almost 40%. Before COVID-19 vaccinations became available, practices put considerable thought into reducing (or eliminating) the amount of time that patients spent in the waiting room. For example, said Dr. Lucarelli, “we now schedule patients with complicated cases later in the clinic, so the entire clinic session does not fall behind due to a patient taking longer than expected.”
His practice also instituted “buffering,” which involves scheduling a more straightforward type of encounter, such as a post-op visit, before and after less predictable encounters, such as a new patient exam. By implementing a multipronged lean overhaul, Dr. Lucarelli has decreased his average total visit time for patients by nearly 40%.
 |
|
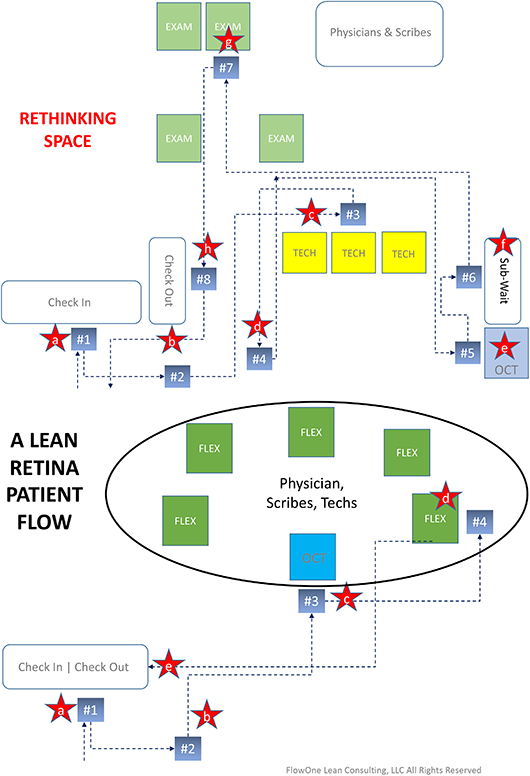
ANALYZING PATIENT FLOW. In this analysis of patient flow at the start of the pandemic (top chart), steps #1 through #8 represent patient motion in the clinic and the red stars represents points where there could be risk of COVID exposure: a) check-in staff; b) other waiting patients; c) tech, other patients (3-foot hallways); d) other waiting patients; e) OCT staff; f) other waiting patients; g) MD and scribe; and h) check-out staff. After reworking patient flow based on lean principles (bottom chart), patient walking distance is reduced by 50% (steps #1 through #4) and there are fewer possibilities of COVID exposure (red stars).
|
Can More Staff Work From Home?
Permitting staff to work remotely not only supports social distancing, it also saves space in the clinic and eliminates some of the operational costs that would be incurred by having them work onsite.
Before the pandemic, Ms. Mangham said that 10 of her staff were already working from home, so practice policies and the technical infrastructure were already in place when the decision was made to make more positions remote. “The moment we had to clear out our call center and billing department—because they were working in a tight, shared collaborative space—we were able to do so. Now we have approximately 20 people working from home, and I do not plan to have these individuals return to the clinic post-COVID. It is unnecessary,” she said.
How scribes can work remotely. UW Health was one of the first academic centers to incorporate virtual scribes, which was a remarkable “game changer,” said Dr. Lucarelli. His scribe is located in Florida and is connected by a secure, HIPAA-compliant audio link. The scribe has access to the patient chart and updates the EHR—from transcribing pertinent patient history and examination information to entering orders and completing after-visit summaries—while Dr. Lucarelli conducts the patient encounter. “This enables me to maintain a more personal and energized, face-to-face encounter with each patient, rather than disengaging while I enter information into the EHR. I preview each visit of the clinic session ahead of time and establish a game plan. This has helped us to become more efficient. Patients have noticed these improvements and have expressed great appreciation,” he said.
At Austin Retina, remote scribing was one of the most helpful of last year’s changes. Austin Retina has also found virtual scribing to be a boon for efficiency and safety. “Some of our physicians wanted to decrease the number of people in the exam room, so they implemented remote scribing,” said Ms. Mangham. “The scribe can be at home, in another office, or in the hallway instead of being in the room with the physician and the patient. The physician simply tells the patient that the scribe is listening to their encounter, and the scribe performs the same duties as if they were present in the room. Making this change was one of the most beneficial adaptations we made in response to the pandemic.”
Incorporating Telemedicine
During the pandemic, telemedicine became an important bridge to patient care for many physicians, even if ophthalmology wasn’t able to utilize it as much as other specialties did. Dr. Goel’s “lightbulb” moment occurred when a patient with flashes and floaters came to the clinic with her daughter early on in the pandemic. “All three of us were wearing masks, and I realized how impersonal the experience had become, so I decided to offer telehealth visits when it is unnecessary for me to see my patients in person—predominantly for consultations and preoperative visits with my laser refractive patients.” He said that he does not charge for this service, and he makes himself available after hours and on weekends to accommodate his patients’ schedules.
Dr. Lucarelli also incorporated telemedicine into his routine for counseling-type visits, primarily, because they are a good fit for this type of interaction. “In oculoplastics, we are often able to observe and assess external conditions remotely as well as gather information and provide education,” he said. “Patients now understand that some of their postoperative care can be conducted remotely. They like the efficiency it provides because they no longer have to travel to the clinic for every visit. I plan to continue to offer this service post-pandemic.” (For tips on telehealth payment, see aao.org/practice-management/telehealth.)
Four Lean Efficiencies
When practices embark on a lean transformation, it helps to start with the low-hanging fruit. The four suggestions below, for example, could be implemented relatively easily.
- Send and receive documents electronically. This saves paper and time.
- Make electronic payments touch-free. Consider taking credit card payments through electronic devices such as Swipesimple or Square to expedite the checkout process.
- Standardize spaces. Arrange every exam room so that equipment is stocked identically, enabling technicians and physicians to quickly find what they need during an exam. Use screening and exam rooms interchangeably, if possible, to avoid moving patients in and out of sub-waiting rooms to minimize exposure and reduce steps.
- Clearly and concisely communicate procedural changes within your clinic. Patients need to understand your current processes and visit expectations to prevent confusion, which can lead to bottlenecks. Convey these messages on your website, via social media, inside the clinic, and at every opportunity available.
|
Create Efficient Physician Flow
As a physician’s available time ultimately determines how many patients can be seen in the clinic, it should never be wasted, said Mr. Suneja. “Constant management, awareness, and communication between the physician and the staff results in efficient use of everyone’s time and talents,” he said. “Staff should ensure that when a physician enters an exam room everything that he or she needs to conduct the exam is easily accessible. When the physician exits the exam room, any pending needs should be passed on before moving on to the next patient.”
He added, “Preventing wasted time for the physician, in between exams, results in less wait time for the next ready patient. This prevents overcrowding in the waiting rooms, and it improves flow through the exam lanes.”
Beyond the Pandemic—How to Maintain a Culture of Innovation
To grow, look beyond the status quo. It is much too easy to become complacent and revert to old habits when things appear to be running smoothly in the clinic. Practices should evaluate their procedures on an ongoing basis and actively seek out areas where improvements can be made. “Choose changes that will be most impactful and are easily achievable by everyone involved, then maintain and build upon your successes,” advised Ms. Mangham, who requires her teams to perform at least four lean trials per year to ensure that they are proactively pursuing more efficient ways of performing their duties.
Meet the Experts
SANJAY D. GOEL, MD A solo practitioner at Goel Vision, which has two locations near Baltimore. Financial disclosures: Carl Zeiss Meditec: C.
ALAN E. KIMURA, MD, MPH President of Colorado Retina Associates and Clinical Associate Professor of Ophthalmology at the University of Colorado Health Sciences Center, both in Denver. Financial disclosures: None.
MARK LUCARELLI, MD, FACS An oculoplastic surgeon at UW Health in Madison, Wis., and medical director of its University Station Eye Clinic, and Dortzbach Professor of Oculofacial Plastic Surgery at UW–Madison. Financial disclosures: None.
STEPHANIE COLLINS MANGHAM, MBA, COA, OCSR CEO at Austin Retina Associates in Austin, Texas. Financial disclosures: Regeneron: C,L.
ANEESH SUNEJA, MBA Lead consultant at FlowOne Lean Consulting, based in Wisconsin. Financial disclosures: FlowOne Lean Consulting: C.
See the disclosure key at www.aao.org/eyenet/disclosures.
Lean Resources
The Lean Practice: A Step-by-Step Guide to Running an Efficient and Profitable Ophthalmic Practice is an AAOE kit that is available in print or as an ebook. It features case studies and downloadable worksheets. Buy it at aao.org/store.
Visit the EyeNet archive. Articles with a lean focus include the following:
Read Mr. Suneja’s guides to lean. He also is coauthor of “Make Your Clinics Flow With Synchrony” (available on Kindle) and author of “Lean Doctors: A Bold and Practical Guide to Using Lean Principles to Transform Healthcare Systems One Doctor at a Time” (ASQ Quality Press; 2010).
Share tips via AAOE’s e-Talk. AAOE members can use the e-Talk listserv to find out how other practices are boosting practice efficiency. Go to aao.org/practice-management/listserv. Not an AAOE member? Join at aao.org/member-services/join-aaoe.
For more on lean, see aao.org/lean.
|
More at AAO 2021
At this year’s annual meeting, make time in your schedule for one or more of these lean events.
SATURDAY, NOV. 13:
- Lean Unexpectedly Proves Its Value During the COVID-19 Pandemic (Event code: 216; senior instructor: Alan E. Kimura, MD, MPH; when: 9:45–11:00 a.m)
- Boost Physician Efficiencies: Creating a Lean Culture With Technology (Event code: 229; senior instructor: Aneesh Suneja, MBA; when: 11:30 a.m.–12:45 p.m.)
SUNDAY, NOV. 14:
- Successful Lean Implementation: The Clinical Manager’s Perspective (Event code: 409; senior instructor: Alan E. Kimura, MD, MPH; when: 9:45–11:00 a.m.)
- Lean for Pediatric Ophthalmology Practices (Event code: 424; senior instructor: Yasmin Bradfield, MD; when: 11:30 a.m.–12:45 p.m.)
- Lean Healthcare Design for Ophthalmology (Event code: 444; senior instructor: Samuel C. Spalding, MD; when: 2:00–3:15 p.m.)
MONDAY, NOV. 15:
- Boost Positive Employee and Patient Experiences Through Lean Process Improvement (Event code: 642; senior instructor: Stephanie Collins Mangham, COA, MBA, OCSR; when: 2:00–3:15 p.m.)
For more information, visit aao.org/programsearch.
|