Download PDF
As with the genomics and proteomics revolutions before it, the study of metabolite levels in the body—known as metabolomics—is promising to give ophthalmic researchers new molecular-level insights into the biological pathways behind some eye diseases.1
Serum metabolites in dry eye disease (DED). One such example came early this year when a study of serum metabolites in a British population-based sample (n = 2,819) found an association between DED and decreased serum androgens.2 Although smaller studies by other groups have suggested a linkage, this is the first hypothesis-free screening study of hundreds of serum metabolites to find the association in a large population cohort, the authors reported.
“The study’s premise was to look for pathways involved in DED and to see if systemic metabolite alterations give us some clue about disease mechanisms in this common problem,” said coauthor Chris Hammond, FRCOphth, the Frost Professor of Ophthalmology at King’s College London. “The exciting discovery that androgen deficiency seems to be associated with DED, along with other work in this area, may lead scientists to developing hormone-based treatments for DED.”
Specifically, the group found a strongly significant metabolome-wide association between dry eye and lower levels of the metabolites androsterone sulfate and epiandrosterone sulfate. Three other molecules involved in androgen metabolism were also lower in the subjects with DED but did not attain metabolome-wide statistical significance.
Considering other eye diseases. There is interest in analyzing tear samples to identify metabolite profiles associated with ocular surface disease, Dr. Hammond said. In other eye diseases, metabolomics would present bigger challenges, he added.
“The difficulty is whether systemic metabolites—typically measured, as in our study, in serum—reflect intraocular diseases such as AMD or glaucoma,” he said. “But certainly, there is evidence of systemic inflammatory changes in AMD; and cataract, for example, has metabolic associations, so these may be possible.”
—Linda Roach
___________________________
1 Tan SZ et al. Eye (Lond). 2016;30(6):773-783.
2 Vehof J et al. Ophthalmology. 2017;124(4):505-511.
___________________________
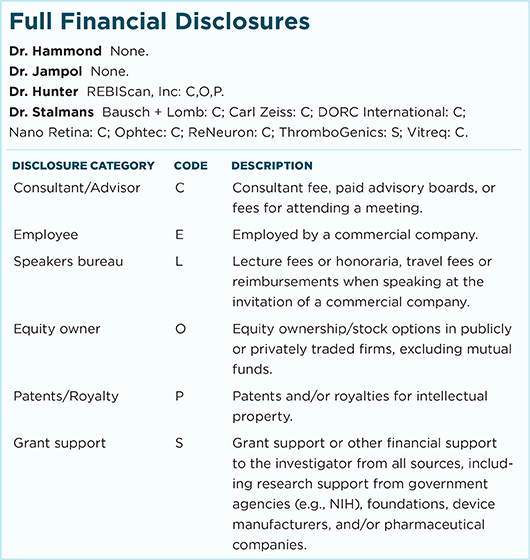
Relevant financial disclosures—Dr. Hammond: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review