Download PDF
This month, News in Review Highlights selected papers from the original papers sessions at AAO 2017. Each was chosen by the session chair because it presents important news or illustrates a trend in the field. Only 4 subspecialties are included here; papers sessions will also be held in 6 other fields. See the Meeting Program, which you’ll find in your meeting bag, or the Mobile Meeting Guide for more information.
A handheld device that delivers tiny electrical pulses inside the nose is proving to be effective for stimulating tear production in dry eye patients.
Edward J. Holland, MD, at the Cincinnati Eye Institute in Ohio, was the medical monitor for the 2 clinical trials of the TrueTear intranasal tear neurostimulator (Allergan). Positive outcomes in the trials led to FDA marketing approval for the device in April.
How it works. Designed to be used daily, the device has 2 soft-tipped prongs that the patient inserts into the superior nasal cavities, slightly anterior, which stimulates tear production, Dr. Holland said. The prongs, which are held in the nose for several seconds, stimulate an ophthalmic branch of afferent trigeminal nerve fibers in the nasal cavity up to 60 times per second with micropulses of 0.7 to 5 milli-Amperes (mA).
Results. “This is a quite effective therapy,” Dr. Holland said. “In both trials, we showed statistically significant increases in Schirmer [scores] both at 1 day and at 180 days.”
The first study was a 1-day randomized crossover trial. Schirmer test scores (mean ± standard deviation) were significantly greater (p < .0001) with active intranasal stimulation than with sham treatment applications (25.3 ± 10.7 mm vs. 9.2 ± 7.3 mm, respectively).
In the second study, an open-label trial, Schirmer scores after 180 days of use also were significantly greater (p < .0001) with intranasal stimulation: 17.3 ± 12.0 mm, compared to 7.9 ± 6.4 mm without stimulation.
No significant adverse events were observed in either study.
Patient satisfaction. “I think a lot of ophthalmologists when they hear about this treatment think that it sounds unusual and the patients won’t use it,” Dr. Holland said. “But patient satisfaction was very, very high. Patients didn’t want to give the device back at the end of the trial.”
| Intranasal Tear Neurostimulation for Subjects With Dry Eye Disease: Results From 2 Pivotal Clinical Trials. When: Sunday, Nov. 12, 2:24-2:31 p.m, during the first cornea original papers session (2:00-3:30 p.m.). Where: Room 255. Access: Free. |
Methods of action. Although aqueous tear deficiency is the sole FDA indication for the prescription-only tear stimulator, other studies have shown that it has additional positive effects, Dr. Holland said.
Researchers have found that the device stimulates all 3 layers of the tear film, Dr. Holland said. “The device stimulates the aqueous layer, and you’ll feel your eyes water. But it also triggers the goblet cells in the conjunctiva to release mucin, and it stimulates the meibomian glands to release meibum,” he said. “You basically improve all 3 layers of the tear film with 1 stimulation, so in theory this could be used for patients with dry eye no matter the etiology.”
Furthermore, in the longer-term trial, patients reported that they needed to use the device less over time, he said. “The longer you’re using the device, the less you [need to] use it, because your ocular surface recovers,” he said.
—Linda Roach
___________________________
Relevant financial disclosures—Dr. Holland: Allergan: C,S.
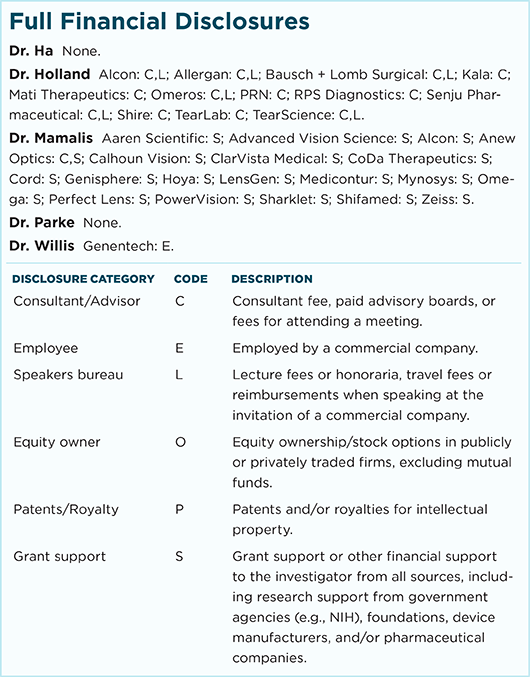
For full disclosures and disclosure key, see below.
More from this month’s News in Review