Download PDF
Problematic IOL Packaging
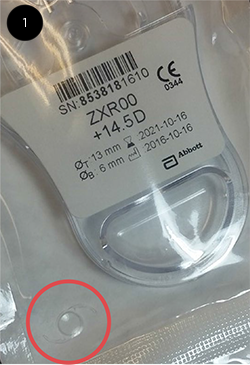 Last week, a patient was scheduled for “premium cataract surgery” using the Tecnis Symfony intraocular lens (IOL) from Abbott Medical Optics (AMO). I opened the sterile packaging to load the lens into its cartridge, but when I opened the cassette, the IOL wasn’t there—the cassette was empty! Thinking this must be an unusual package that had somehow slipped through quality control, I asked for another lens. Fortunately, we had a backup in the correct power. Again, I opened the peel pack so I could load the lens prior to beginning the surgery. Imagine my surprise when this second cassette was empty, too! My patient was prepped and draped, expecting a new depth-of-focus IOL. The OR staff were all in place, ready for the surgery to commence. Do I call for another premium lens? Should I just default to a standard monofocal lens? Or, do I delay the case until we can order more Symfony lenses that actually contain the IOL? Out of frustration, I reexamined all the lens packaging again and discovered the IOL! It was not in the cassette—it was nearly hidden, floating in the corner of the peel pack (Fig. 1). The IOL appeared to be unscathed, and I retrieved it, loaded it into the cartridge, and proceeded with the case. And later, when I examined the packaging that I had opened earlier, that IOL also was discovered floating freely in its peel pack. On further examination, it appeared that the cassette does not have a locking mechanism to keep the IOL in position. Likely a redesign of the Symfony cassette is warranted to properly secure the IOL. Until this time, surgeons should be aware that the IOL could fall out of its cassette and be sure to thoroughly check the peel pack if the lens appears to be absent.
Last week, a patient was scheduled for “premium cataract surgery” using the Tecnis Symfony intraocular lens (IOL) from Abbott Medical Optics (AMO). I opened the sterile packaging to load the lens into its cartridge, but when I opened the cassette, the IOL wasn’t there—the cassette was empty! Thinking this must be an unusual package that had somehow slipped through quality control, I asked for another lens. Fortunately, we had a backup in the correct power. Again, I opened the peel pack so I could load the lens prior to beginning the surgery. Imagine my surprise when this second cassette was empty, too! My patient was prepped and draped, expecting a new depth-of-focus IOL. The OR staff were all in place, ready for the surgery to commence. Do I call for another premium lens? Should I just default to a standard monofocal lens? Or, do I delay the case until we can order more Symfony lenses that actually contain the IOL? Out of frustration, I reexamined all the lens packaging again and discovered the IOL! It was not in the cassette—it was nearly hidden, floating in the corner of the peel pack (Fig. 1). The IOL appeared to be unscathed, and I retrieved it, loaded it into the cartridge, and proceeded with the case. And later, when I examined the packaging that I had opened earlier, that IOL also was discovered floating freely in its peel pack. On further examination, it appeared that the cassette does not have a locking mechanism to keep the IOL in position. Likely a redesign of the Symfony cassette is warranted to properly secure the IOL. Until this time, surgeons should be aware that the IOL could fall out of its cassette and be sure to thoroughly check the peel pack if the lens appears to be absent.
I am currently working with AMO to resolve this via their product safety and compliance team.
J.T. Kavanagh, MD
Seguin, Texas
Response From AMO
In response to the above letter, Abbott Medical Optics Inc. (AMO) can confirm that the complaint raised in his letter was investigated, the root cause of the issue was identified, and corrective actions were implemented in the manufacturing processes to prevent this issue from occurring in the future. We reached out and spoke directly to the surgeon when the matter was brought to our attention. No patient injury occurred in connection with this complaint.
At AMO, we are fully dedicated to delivering quality products and take patient safety and customer complaints very seriously. I, and my colleagues around the world, strive every day to help transform lives by providing high-quality, innovative surgical technologies that help improve the way people see. If you have product complaints or adverse events to report regarding any AMO product, please call our customer service line at 877-266-4543.
We thank the ophthalmic community for their continued partnership.
Tom Frinzi
President, Johnson & Johnson Vision, Surgical Platform
(Please note that Abbott Medical Optics Inc. is now a member of the Johnson & Johnson Family of Medical Device Companies)
IOP During Sleep
We read with interest your recent article “Update on 24-Hour IOP Monitoring” (Clinical Update, January), which discussed assessing intraocular pressure (IOP) during sleep. People are asleep for roughly 25%-30% of their lives. The character of the IOP during sleep has not been studied until recently, as there were no suitable devices to make these measurements. Previous studies of IOP during sleep employed standardinstruments that were used just after patients were awakened. The contact lens–based sensor detects limbal strain (Triggerfish) and is an elegant concept utilized by Dr. Mansouri’s group1 and Dr. Quigley’s group2 to estimate the IOP while the subjects’ eyes were closed and while they were in standard sleeping postures.
Using an ocular pressure estimator, a technology based upon a different physics principle, we estimated IOP while the subjects’ eyes were closed and their dependent eye made contact with a pillow.3,4 We found substantial elevations in estimated IOP in the eye in contact with the pillow, often to 40-100 mm Hg for short periods of time while the subjects positioned themselves in their usual sleep position. Such large intermittent occult elevations of IOP may be clinically relevant, considering that every mm Hg of IOP reduction from ocular hypotensive treatment is beneficial.5 We share in the excitement of looking at this previously unstudied interval of risk, as sleep-related elevations of IOP over a lifetime are very likely to affect the onset and trajectory of many other conditions—not only glaucoma but also diabetic retinopathy, the conversion of dry to wet macular degeneration, the production of intraocular venous occlusions, and the oculocardiac reflex in infants and sudden infant death syndrome.4
Michael S. Korenfeld, MD
Washington, Mo.
___________________________
1 Mansouri K et al. Invest Ophthalmol Vis Sci. 2012;53(13):8050-8056.
2 Flatau A et al. JAMA Ophthalmol. 2016;134(4):375-382.
3 Korenfeld MS et al. Clin Ophthalmol. 2016;10:71-77.
4 Korenfeld MS et al. Clin Ophthalmol. 2016;10:343-357.
5 Leske MC et al. Arch Ophthalmol. 2003;121(1):48-56.
Further Thoughts on Globe Flattening in Astronauts
We read with interest “What Flattens Astronauts’ Eyes?” (News in Review, February). Researchers at the University of Miami have found evidence to support a microgravity-induced buildup of cerebrospinal fluid (CSF) in the orbit and ventricles in the brain during long-duration space flight (LDSF) as a possible mechanism for these findings. However, the potential role of CSF in the optic nerve (ON) sheaths and the resultant findings of globe flattening and visual changes have been investigated by other researchers both prior to and following Dr. Alperin’s excellent research. NASA researchers and consultants from across the spectrum of neuroscience (including ophthalmology, neurology, neuroradiology, and neurosurgery) have been actively involved in this fascinating area of research for many years now, and much has been published in the peer-reviewed literature.1-6 We wish to share with you some of that additional prior work as well as to update your readers on new information.
In 2011, a report from the Space Medicine Division of the National Aeronautics and Space Administration (NASA) proposed that elevated intrasheath CSF pressure was a possible mechanism that might explain disc edema, globe flattening, hyperopic shifts in refraction, and other findings reported in astronauts during and after LDSF.1 Elevated intrasheath CSF pressure was thought to cause the subarachnoid compartment to exert an anterior force that indents the posterior sclera, resulting in posterior globe flattening, choroidal folding, and axial shortening.1 In this article, it was proposed that the rise in intrasheath CSF pressure and volume resulted from 2 possible mechanisms or perhaps a combination of the 2. One possibility was that a rise in intracranial pressure (ICP) occurred during LDSF as a result of fluid shifts. In this scenario, CSF would be propagated down the ON sheaths toward the globes with a resultant rise in orbital ON sheath pressure. Interestingly, astronauts with disc edema have not complained of severe headaches, transient visual obscurations, or other symptoms usually associated with high ICP on Earth. However, moderately elevated postmission ICP has been documented on several lumbar puncture opening pressures (LPOP) in astronauts with disc edema and globe flattening. One of these measurements of ICP was as high as 28.5 cm H20, suggesting increased ICP as an etiology of the findings. An alternate theory proposed that there was a rise in ON sheath CSF pressure, as a result of ON sheath compartmentalization within the orbit, with or without a rise in ICP.1-5 In support of this theory, an astronaut who returned from LDSF with unilateral grade 1 disc edema had a normal LPOP of 18 cm H20 8 days after landing.2 He also had the unilateral loss of previously visible spontaneous venous pulsations during space flight in the eye with the disc swelling that continued to be absent 21 months after his return to Earth, suggesting a long-term rise in sheath pressure.3
Another more recent study documented optic disc edema and globe asymmetry for 6 months following a LDSF despite LPOPs of 22 cm and 16 cm H20 at 1 week and 1 year after flight, respectively.4 These LPOPs are not believed to be sufficiently high to cause or maintain disc edema. Thus, these findings suggest that increased ICP alone, at least in these astronauts, may not be the sole cause of the globe flattening or disc edema.
In summary, although the precise mechanism for these findings in astronauts remains unknown, continued research from multiple neuroscience clinicians and researchers strongly suggests that increased ON sheath CSF pressure and volume changes are responsible for the disc edema, globe flattening, hyperopic shifts, and other findings during and after LDSF.1-5 A 2012 report by Dr. Kramer using 3T magnetic resonance imaging of the orbit and brain also confirmed posterior globe flattening, ON protrusion, and ON sheath changes in astronauts returning from space flight.6 In addition, it should be noted that the term visual impairment intracranial pressure syndrome (VIIP), as mentioned by Dr. Alperin, has recently been changed by NASA to spaceflight associated neuro-ocular syndrome (SANS), as this may be a more appropriate term. Dr. Alperin’s research offers further confirmatory evidence, in support of previous NASA studies, regarding the role of CSF fluid in the production of globe flattening and hyperopic visual changes during and after LDSF.
Thomas H. Mader, MD COL(R), Cooper Landing, Alaska
C. Robert Gibson, OD, Houston
Andrew G. Lee, MD, Houston
Prem S. Subramanian, MD, PhD, Aurora, Colo.
Neil R. Miller, MD, Baltimore
Larry A. Kramer, MD, Houston
___________________________
1 Mader TH et al. Ophthalmology. 2011;118(10):2058-2069.
2 Mader TH et al. J Neuroophthalmol. 2013;33(3):1249-1255.
3 Mader TH. J Neuroophthalmol. 2015;35(2):226-227.
4 Mader TH et al. J Neuroophthalmol. 2016 Dec 5. doi:10.1099/WNO.00000000000000467. [Epub ahead of print]
5 Lee AG et al. J Neuroophthalmol. 2016;36(1):85-91.
6 Kramer LA et al. Radiology. 2012;263(3):819-827.