Visual System History Assessment
Relevant family history regarding eye disorders (cataracts, strabismus, amblyopia, and refractive error), eye surgery, and the use of glasses during childhood in parents or siblings should be explored. Parents’ observations are also valuable in the history and review of systems. Questions that can be asked include:
-
Do your child’s eyes appear unusual?
-
Does your child seem to see well?
-
Does your child exhibit difficulty with near or distance vision?
-
Do your child’s eyes appear straight or do they seem to cross?
-
Do your child’s eyelids droop or does one eyelid tend to close?
-
Has your child ever had an eye injury?
Ocular Examination
The ocular examination consists of the external examination, pupil examination, red reflex testing to assess ocular media, the examination of the ocular fundus by using ophthalmoscopy, and an assessment of visual function.
External Examination (Lids/Orbit/Conjunctiva/Cornea/Iris)
External examination of the ocular structures consists of a penlight evaluation of the eyelids, conjunctiva, sclera, cornea, and iris. Detection of abnormalities, such as ptosis, nonresolving conjunctivitis, or the presence of cloudy or enlarged corneas and/or photophobia, necessitates timely referral to an eye care specialist appropriately trained to treat children. Nasolacrimal duct obstruction that has not resolved by 1 year of age also should lead to referral. Thyroid disease can manifest by increased visibility of the superior cornea caused by eyelid retraction.
Red Reflex Testing
Red reflexes from the retinas can be used by the physician to great advantage. The red reflex test, or Bruckner test if performed binocularly, is used to detect opacities in the visual axis, such as a cataract or corneal abnormality, as well as abnormalities in the posterior segment, such as retinoblastoma or retinal detachment. The examiner also may detect subtle differences in the red reflex between the eyes, consistent with the presence of strabismus or refractive errors. The inequality of the red reflection or the interference with the red reflection can be noted in various conditions (Fig 1).

Red reflex testing should be performed in a darkened room (to maximize pupil dilation). Eye drops to further dilate the pupils are not necessary. The direct ophthalmoscope is set on “0,” and while viewing through it at a distance of approximately arm’s length from the child, both pupils are evaluated simultaneously as the child looks at the light. To view more detail, the examiner can move closer to the child to assess each eye individually. The observed red reflexes can be compared and should be a light orange-yellow in color in lightly pigmented eyes or a dark red in darkly pigmented brown eyes. If normal, the 2 red reflexes should be identical in color, brightness, and size. A bright white or yellow reflex or, conversely, a dull or absent red reflex can be an indication of a significant abnormality that necessitates further evaluation by a pediatric ophthalmologist, or if unavailable, a comprehensive ophthalmologist or optometrist with specialized interest in the treatment of children, and who uses cycloplegia (dilating drops) as part of his or her routine evaluation. Because there is often considerable variation in the qualitative nature of the red reflex among patients without eye abnormalities, the frequent, routine assessment of the red reflex will help the primary care physician better distinguish an abnormality of the reflex from a normal one.
Pupil Examination
Both pupils should be equal, round, and equally reactive when light is directed toward either eye. Asymmetric responses to light may indicate visual system dysfunction. Moreover, asymmetry of pupil shape or difference in diameter greater than 1 mm can often be attributable to an ocular injury or disease or to a neurologic disorder. Differences in pupil size less than 1 mm can occur normally and are generally benign unless associated with ptosis or an ocular motility deficit.
Ocular Alignment and Motility Assessment
The assessment of ocular alignment in the preschool- and early school-aged child is also important. The development of strabismus in children may occur at any age and, although often isolated, may also represent serious orbital, intraocular, or intracranial disease.
The corneal light reflex test and the cover test are each useful in identifying the presence of strabismus as well as in differentiating true strabismus from pseudostrabismus.
The corneal light reflex test (i.e., Hirschberg test) is performed with a penlight directed onto the child’s face from arm’s length away and by observing the symmetrical location of the white pinpoint light reflexes while the child gazes at the light. Normally, these reflexes fall symmetrically in or near the center of the pupils. An abnormal response occurs when the reflex in one eye is centered in the pupil while the reflex in the opposite eye is displaced nasally, temporally, or vertically away from the pupil center (Fig 1). This asymmetry of the reflexes typically indicates the presence of strabismus.
The cover test should be performed while the child fixates on a small, interesting target, such as a small toy or sticker on a tongue depressor. The bright beam of a penlight does not provide a comfortable target and does not adequately stimulate accommodation (focusing). As the child attends to the target, each eye is alternately covered. A shift in an eye’s alignment as it assumes fixation onto the target is a possible indication of strabismus.
Strabismus in the neonatal period is not unusual, and intermittent strabismus is often a normal finding in early infancy. However, constant horizontal strabismus that persists after 4 months of age does not resolve spontaneously.5 Thus, any child older than 4 months with strabismus should be referred for evaluation.
Pseudostrabismus is the appearance of crossed eyes (esotropia) attributable to the presence of prominent epicanthal skin folds that cover the medial portion of the sclera on 1 or both eyes, giving the false impression of esotropia. The inability to differentiate strabismus from pseudostrabismus also necessitates referral.
Finally, the presence of unusual eye movements in an infant or young child may indicate nystagmus or a similar disorder and often indicates decreased vision or neurologic dysfunction. Nystagmus does not resolve spontaneously and often indicates afferent visual system dysfunction or neurologic disease and necessitates further evaluation by either an ophthalmologist or neurologist.
Ophthalmoscopy
Use of the direct ophthalmoscope in older, cooperative children serves to visualize structures in the back of the eye, such as the optic nerve, retinal blood vessels, and central retina (fovea). To properly visualize these structures, the child looks into the distance at a target of interest. The ophthalmoscope is dialed to a +10 lens and the examiner focuses on the pupil from ∼3 inches away. The examiner then gradually moves as close to the eye as possible while sequentially dialing less lens power until retinal vessels come into focus. These vessels can be followed to identify and view the optic nerve. The normal optic nerve has a yellow-pink color and is generally flat. To view the foveal reflex, the child is asked to look directly at the light of the ophthalmoscope. The normal foveal reflex should appear bright and sharp. Retinal hemorrhages can be observed after a normal vaginal delivery but are also the harbinger of severe child abuse; a swollen optic nerve may be an indicator of increased intracranial pressure.
Assessment of Visual Acuity in Preverbal Children
The assessment of visual function in this very young age group is best accomplished by evaluating the child’s ability to fixate on and follow an object held before the child. A standard assessment strategy is to determine whether each eye can independently fixate on the object, maintain fixation on it for a short period of time, and then follow it as it is moved in various directions. The child should be awake and alert for this testing, and the targeted object should be a toy or something of interest to the child. Disinterest or poor cooperation can mimic a poor vision response. This assessment should first be performed binocularly and then repeated with each eye alternately covered. If poor binocular fixation and following behavior is noted after 3 months of age, an ocular or neurologic abnormality may be present. Similarly, asymmetry in responses between the 2 eyes in children of any age necessitates further evaluation.
Assessment of Visual Acuity in Older Children
Children who are old enough to delineate objects on a wall-mounted or handheld eye chart can provide a direct measurement of visual acuity. For some children, this may be accomplished as young as 3 years, but for the typical healthy child, an accurate visual acuity can be achieved with a high degree of success at 4 years and older. Eyes should be tested monocularly, ensuring that the child does not peek with the fellow eye.
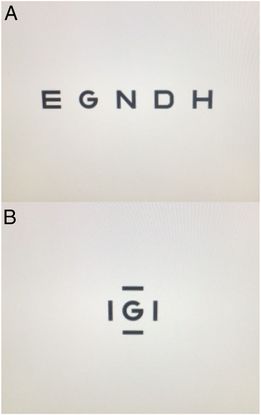
With traditional visual acuity screening, the selection of age-appropriate shapes or letters and specific testing methods is crucial in obtaining the most accurate screening results. Many children can identify optotypes (figures or a selection of distinct letters formatted on chart lines or presented singly on individual cards) by 4 years of age. Eye charts using lines of optotypes or matching cards with lines (crowding bars) around each optotype provide the most accurate assessments of visual acuity (Fig 2). Using cards with single optotypes but without crowding bars can overestimate visual acuity. Crowding bars surround an optotype and make individual letters more difficult to recognize by an amblyopic eye, thus increasing the sensitivity to detect amblyopia (Fig 2). Accurate assessment of visual acuity, therefore, is best accomplished by using a line of symbols or symbols with crowding bars around them.
The currently preferred optotypes are the LEA or HOTV symbols, although other new picture optotype acuity tests are under development.6,7 Allen figures, Lighthouse characters, and the Sail Boat Chart are not standardized and are no longer recommended for use, nor are the Tumbling E or Landolt C charts, because a child of preschool age may not yet have developed the ability to express the orientation of these optotypes. HOTV symbols are easier for the young child to understand, as they are symmetric and not subject to letter reversal. With the examiner pointing to a symbol with a finger under it, a timid child can point to the optotypes that he or she recognizes on a card with similar symbols; this allows the child to effectively offer nonverbal responses during testing. Once a child can distinguish letters, a chart with letter optotypes should be used. Although the traditional Snellen chart remains in wide usage, Sloan letter charts present letters in a standardized fashion and should be used for acuity testing if they are available.
Screening Process
Large optotypes at the top of an eye chart or on handheld cards are first reviewed with the child with both eyes open to help the child understand the test. After this review, 1 eye is occluded (preferably by an occlusive patch or tape) and lines of optotypes or cards with single crowded optotypes (i.e., the figure is surrounded by bars on all 4 sides) are presented to each eye separately. Effective occlusion, such as with tape or an occlusive patch of the eye not being tested, is important to eliminate the possibility of peeking.
Threshold Line Evaluation
The time-honored method of testing visual acuity has been to ask the child to start at the top of an eye chart and continue reading down each line until he or she recites the smallest line of optotypes discernable with each eye tested separately. This method is called “threshold” acuity testing and remains a common method of acuity testing. It enables one to identify the best level of visual acuity in each eye. Thus, children with near-normal acuity who still have a mild difference in acuity between each eye can be detected. However, threshold line evaluation can be sufficiently time-consuming to result in loss of attention from a young subject.
Critical Line Evaluation
Young children, even those with normal vision, are frequently unable to attend sufficiently to small optotypes and identify them. “Critical line” screening is an effective alternative to threshold testing for identifying children with potentially serious vision concerns and can be more quickly administered than can screening by using threshold testing. The “critical line” is the age-dependent line a child is expected to see normally and pass. For screening purposes, it is unnecessary to measure acuity below the age-specific critical line to pass the test. The critical line to pass screening becomes smaller as age increases. Most eye charts present 4 to 6 optotypes per line, and passing the screening requires the child to correctly answer a simple majority of the optotypes present on the critical line appropriate for his or her age as follows:
-
Ages 36 through 47 months: If attempted at this age, the critical line to pass screening is the 20/50 line
-
Ages 48 through 59 months: The critical line to pass screening is the 20/40 line
-
Ages 60 months and older: The critical line to pass screening is the 20/30 line (or the 20/32 line on some charts)
Establishing an Effective Screening Environment and Methodology
It is important that the screening area be conducive for assessing visual acuity and that proper technique is used to promote accurate screening. It is important that screening personnel be trained to recognize and avoid pitfalls that reduce the accuracy of visual acuity screening. Accurate screening of visual acuity requires dedicated and skilled staff members.
-
A well-illuminated area free from distraction is important. A quiet examination room or hallway is generally sufficient for this purpose.
-
An appropriate testing distance must be used. For children up to 5 years of age, especially when pictorial optotypes are used, this distance should be set at 10 feet rather than 20 feet as a standard. This shorter distance helps to enhance interaction between the child and the individual administering the screening without decreasing the accuracy of screening results. Indeed, current standardized preschool eye charts are typically calibrated for use at 10 feet. For children 6 years and older for whom a letter chart is used, the test distance may be appropriately set at either 10 feet or at the common standard of 20 feet, as long as the chart is properly calibrated for use at that distance.
Increasingly, screening methods using short testing distances are becoming available in the form of handheld optotypes used at a testing distance of 5 feet8 or as computer, tablet, or smart phone–based models with testing distances within 1 to 2 feet. Although the accuracy of screening visual acuity at these shorter distances has not yet been validated in large population-based studies, the use of these methods can fit well into small clinical work areas. One computer-based application, available from the Jaeb Center for Health Research, is specifically for use by nonophthalmic health care professionals. The Jaeb Visual Acuity Screener incorporates all current screening guidelines and is available free of charge for download and unlimited use at http://pedig.jaeb.org/JVAS.aspx.
-
3. It is important to recognize that children with visual impairment may inaccurately pass a vision screening if they peek around an incompletely covered eye or if they are able to correctly guess when only 2 or 3 optotype choices are presented. Use of an adhesive patch over the nontested eye is recommended. Visually impaired children may become uncooperative during an examination; such behavior should be considered a possible indicator of poor visual function.
-
4. The use of validated and standardized optotypes and acuity charts is important for an accurate assessment of vision. For this reason, only the LEA symbols and HOTV characters are recommended for preschool vision screening at this time. Other optotypes are not well validated in the screening environment.
-
5. Every effort should be made not to isolate shapes or letters inadvertently on a line with a finger or cover to “help” a struggling child. If performed in this manner, the visual acuity result may be made falsely elevated by blocking out the natural crowding inherent in open lines of letters. If single optotypes are presented, they should include “crowding bars.”
-
6. Screening visual acuity to the child’s threshold (ie, best possible acuity) may provide a less accurate result than testing to the age-appropriate critical line for that child. Critical line testing is an appropriate alternative to threshold testing, requires less time to administer, and may provide a more accurate screening assessment of a child’s visual function.
Incorporating these concepts into clinical practice offers a quick and reliable assessment of visual acuity in young children. To assist pediatricians and primary care physicians, the American Association for Pediatric Ophthalmology and Strabismus has developed a Vision Screening Kit designed specifically for young children that incorporates these important concepts. It is available commercially and can be purchased from the AAP.
For healthy children 6 years and older, testing of visual acuity using optotype-based vision charts at 10 or 20 feet remains the preferred method for screening and should be repeated every 1 to 2 years (Table 1).
Although barriers to its use exist, a level-1 Current Procedural Terminology (CPT) code, 99173, has been established for visual acuity screening and is available to primary care physicians to seek payment for this testing.
Instrument-Based Screening Techniques
Instrument-based screening is endorsed by the AAP2 and by the US Preventive Services Task Force as a valid method for screening very young children.9 A recent randomized, controlled, multicentered crossover study demonstrated photoscreening to be superior to direct testing of visual acuity for screening well children ages 3 to 6 years in the pediatric office.10 If available, instrument-based screening can be attempted beginning at age 12 months,11 and a previous study has demonstrated better eventual outcomes for children undergoing their first photoscreening before 2 years of age.12
Instrument-based screening can be relatively quick and requires less attention from the child compared with traditional visual acuity screening. Screening instruments identify optical and physical characteristics that indicate the presence of ocular conditions known to cause amblyopia. Similar to the code for visual acuity screening, a level-1 CPT code, 99174, has been assigned to photoscreening and enables the primary care physician to seek payment for its use. CPT codes 99173 and 99174 are specific for visual acuity screening and photoscreening, respectively.
Two types of instrument-based vision screening are now available for use in ambulatory care settings. Although neither type provides a direct assessment of visual acuity, both identify ocular risk factors that can lead to early vision loss in children. Once children can read an eye chart easily, optotype-based acuity should supplement instrument-based testing. The actual age for this is not yet well established and likely varies depending on the child.
The most common ocular abnormalities seen during the early childhood years are strabismus, anisometropia, and a high magnitude of uncorrected refractive errors: hypermetropia, myopia, and astigmatism. The American Association for Pediatric Ophthalmology and Strabismus has developed refractive criteria to help primary care physicians appreciate the levels of refractive error known to increase risk of amblyopia (Table 2).13 Referral criteria that best detect these amblyopia risk factors may vary depending on the screening instrument used and the desired levels of sensitivity and specificity.
Photoscreening devices identify optical characteristics of the eyes to estimate refractive error, media clarity, ocular alignment, and eyelid position. Abnormalities in these characteristics constitute risk factors for the presence or development of amblyopia. Photoscreening has been shown to have high sensitivity and specificity in community and office settings.14–20 Photoscreening instruments assess both eyes simultaneously and the images can be interpreted by trained operators, by a central reading center, or with computer software.
Autorefraction instruments, like photoscreeners, also are useful for screening young children.21,22 Handheld autorefractors use optical methods to estimate the refractive error of each eye, 1 eye at a time, and as such, are limited in their ability to detect strabismus in the absence of an abnormal refractive error. However, autorefractors remain useful in detecting anisometropia in the absence of strabismus, which is the most common cause of amblyopia undetected at an early age.
Instrument-based devices using technology based on visual evoked potentials23 and retinal birefringence24 are currently in development and may provide additional means to assess visual acuity and ocular health in young children.
For all instrument-based devices, the sensitivity and specificity to detect an ocular abnormality has been carefully considered by their manufacturers. Typically, when a high sensitivity (ie, high rate of detection of at-risk children) is chosen, an increase in overreferrals (ie, low specificity) results. Conversely, when a high specificity is set, there is often a low sensitivity (ie, reduced detection of at-risk children). Given these factors, the referral criteria can be adjusted for many instruments on the basis of the child’s age and desired levels of sensitivity and specificity.
Lead Authors
Sean P. Donahue, MD, PhD, FAAP
Cynthia N Baker, MD, FAAP
AAP Committee on Practice and Ambulatory Medicine, 2014–2015
Geoffrey R. Simon, MD, FAAP, Chairperson
Cynthia N Baker, MD, FAAP
Graham Arthur Barden, III, MD, FAAP
Oscar W. “Skip” Brown, MD, FAAP
Jesse M. Hackell, MD, FAAP
Amy Peykoff Hardin, MD, FAAP
Kelley E. Meade, MD, FAAP
Scot B. Moore, MD, FAAP
Julia Richerson, MD, FAAP
Staff
Elizabeth Sobczyk, MPH, MSW
AAP Section on Ophthalmology Executive Committee, 2014–2015
Sharon S. Lehman, MD, FAAP, Chairperson
David B. Granet, MD, FAAP
Geoffrey E. Bradford, MD, FAAP
Steven E. Rubin, MD, FAAP
R. Michael Siatkowski, MD, FAAP
Donny Won Suh, MD, FAAP
David B. Granet, MD, FAAP, Immediate Past Chairperson
Liaisons
Noelle S. Matta, CO, COT – American Association of Certified Orthoptists
Christie Morse, MD, FAAP – American Association of Pediatric Ophthalmology and Strabismus
Pamela E. Williams, MD, FAAP – American Academy of Ophthalmology
Gregg T. Lueder, MD, FAAP – American Academy of Ophthalmology Council
C. Gail Summers, MD – American Academy of Ophthalmology
George S. Ellis, Jr, MD, FAAP – Section Historian
Staff
Jennifer G. Riefe, MEd
American Academy of Ophthalmology
American Association for Pediatric Ophthalmology and Strabismus
American Association of Certified Orthoptists
Acknowledgments
The writing committee and lead author thank Drs James B. Ruben, MD, FAAP, and Geoffrey E. Bradford, MD, FAAP, for assistance with drafting and editing this document.
References
- American Academy of Pediatrics. Section on Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics. 2015, In press
- Miller JM, Lessin HR; American Academy of Pediatrics Section on Ophthalmology; Committee on Practice and Ambulatory Medicine, American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Instrument-based pediatric vision screening policy statement. Pediatrics. 2012;130(5):983–986pmid:23109679 Abstract/FREE Full Text
- Committee on Practice and Ambulatory Medicine, Section on Ophthalmology. American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003;111(4 pt 1):902–907pmid:12671132 Abstract/FREE Full Text
- American Academy of Pediatrics, Section on Ophthalmology,American Association for Pediatric Ophthalmology And Strabismus, American Academy of Ophthalmology, American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics. 2008;122(6):1401–1404pmid:19047263 Abstract/FREE Full Text
- Birch E, Stager D, Wright K, Beck R; Pediatric Eye Disease Investigator Group. The natural history of infantile esotropia during the first six months of life. J AAPOS. 1998;2(6):325–328, discussion 329pmid:10532717 CrossRefMedline
- Mercer ME, Drover JR, Penney KJ, Courage ML, Adams RJ. Comparison of Patti Pics and Lea Symbols optotypes in children and adults. Optom Vis Sci. 2013;90(3):236–241pmid:23376895 CrossRefMedline
- Shah N, Laidlaw DA, Rashid S, Hysi P. Validation of printed and computerised crowded Kay picture logMAR tests against gold standard ETDRS acuity test chart measurements in adult and amblyopic paediatric subjects. Eye (Lond). 2012;26(4):593–600pmid:22193878 CrossRefMedlineWeb of Science
- Kulp MT; Vision in Preschoolers Study Group. Findings from the Vision in Preschoolers (VIP) study. Optom Vis Sci. 2009;86(6):619–623pmid:19417714 CrossRefMedline
- US Preventive Services Task Force. Vision screening for children 1 to 5 years of age: US Preventive Services Task Force Recommendation statement. Pediatrics. 2011;127(2):340–346pmid:21282267 Abstract/FREE Full Text
- Salcido AA, Bradley J, Donahue SP. Predictive value of photoscreening and traditional screening of preschool children. J AAPOS. 2005;9(2):114–120pmid:15838437 CrossRefMedlineWeb of Science
- Longmuir SQ, Boese EA, Pfeifer W, Zimmerman B, Short L, Scott WE. Practical community photoscreening in very young children. Pediatrics. 2013;131(3). Available at: www.pediatrics.org/cgi/content/full/131/2/e764pmid:23400603
OpenUrlAbstract/FREE Full Text
- Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal photoscreening for amblyogenic factors and outcomes in amblyopia treatment: early objective screening and visual acuities. Arch Ophthalmol. 2008;126(4):489–492pmid:18413517
OpenUrlCrossRefMedlineWeb of Science
- Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB; POS Vision Screening Committee. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17(1):4–8pmid:23360915 CrossRefMedlineWeb of Science
- Matta NS, Singman EL, Silbert DI. Performance of the plusoptiX S04 photoscreener for the detection of amblyopia risk factors in children aged 3 to 5. J AAPOS. 2010;14(2):147–149pmid:20451857 CrossRefMedline
- Longmuir SQ, Pfeifer W, Leon A, Olson RJ, Short L, Scott WE. Nine-year results of a volunteer lay network photoscreening program of 147 809 children using a photoscreener in Iowa. Ophthalmology. 2010;117(10):1869–1875pmid:20656350 CrossRefMedlineWeb of Science
- Bloomberg JD, Suh DW. The accuracy of the plusoptiX A08 photoscreener in detecting risk factors for amblyopia in central Iowa. J AAPOS. 2013;17(3):301–304pmid:23791414 CrossRefMedline
- Ransbarger KM, Dunbar JA, Choi SE, Khazaeni LM. Results of a community vision-screening program using the Spot photoscreener. J AAPOS. 2013;17(5):516–520pmid:24160974 CrossRefMedline
- Arnold RW, Arnold AW, Armitage MD, Shen JM, Hepler TE, Woodard TL. Pediatric photoscreeners in high risk patients 2012: a comparison study of Plusoptix, Iscreen and SPOT. Binocul Vis Strabolog Q Simms Romano. 2013;28(1):20–28pmid:23521032 Medline
- Garry GA, Donahue SP. Validation of Spot screening device for amblyopia risk factors. J AAPOS. 2014;18(5):476–480pmid:25266832 CrossRefMedline
- Peterseim MMP, Papa CE, Wilson ME, et al. The effectiveness of the Spot Vision Screener in detecting amblyopia risk factors. J AAPOS. 2014;18(6):539–542pmid:25498463 CrossRefMedline
- Rowatt AJ, Donahue SP, Crosby C, Hudson AC, Simon S, Emmons K. Field evaluation of the Welch Allyn SureSight vision screener: incorporating the vision in preschoolers study recommendations. J AAPOS. 2007;11(3):243–248pmid:17140828 CrossRefMedline
- Silverstein E, Lorenz S, Emmons K, Donahue SP. Limits on improving the positive predictive value of the Welch Allyn SureSight for preschool vision screening. J AAPOS. 2009;13(1):45–50pmid:18976944 CrossRefMedline
- Simon JW, Siegfried JB, Mills MD, Calhoun JH, Gurland JE. A new visual evoked potential system for vision screening in infants and young children. J AAPOS. 2004;8(6):549–554pmid:15616502 CrossRefMedlineWeb of Science
- Loudon SE, Rook CA, Nassif DS, Piskun NV, Hunter DG. Rapid, high-accuracy detection of strabismus and amblyopia using the pediatric vision scanner. Invest Ophthalmol Vis Sci. 2011;52(8):5043–5048pmid:21642624 Abstract/FREE Full Text
Copyright © 2016 by the American Academy of Pediatrics