Eyelid and Canalicular Lacerations
Lesions of the eyelids and ocular adnexa are a frequent manifestation of facial trauma, especially in children. Specifically, canalicular lacerations are more often found in children than adults. These are most commonly caused by dog bites and are more likely to occur within the first decade of life.1–3 Although there are similarities in management between adults and children, there are also important differences.
Injuries to the eyelids can be classified as either blunt or penetrating and marginal or extramarginal. Do a thorough exam including evaluation of the following:
- lid margin and canalicular system
- canthal tendon integrity
- presence or absence of foreign bodies
- nerve or muscle damage
- extent of tissue loss
Additionally, evaluate the globe and fundus to rule out any intraocular pathology.
If the eye exam shows pathology pressing for repair, postpone management of the eyelid injury, placing plastic occlusive dressing with copious corneal lubrication until the repair is completed.
Often eyelid edema and ecchymosis are the common presenting signs. If eyelid edema is significant, opening the eye for exam can be difficult, but can be aided by a Desmarres retractor or bent paper clip.
Examine fornices for debris or other foreign bodies.
Assess the levator muscle because failure to repair injury can result in ptosis.
A crease, if seen despite swelling, can indicate levator attachment, whereas prolapsed fat can point to damage. Levator function can be assessed by firmly pressing on the brow and measuring the distance between the upper eyelid on maximal downgaze and maximal upgaze, however, this is often very difficult in children and infants, and normative data has not been determined.
Rounding of the medial or lateral canthus indicates possible canthus rupture, and a medially located eyelid laceration can involve the canalicular system and might require probing and irrigation. Lastly, orbital fat protrusion can be an indication of orbital septum perforation by a foreign body.
Managing eyelid lacerations in adults can often be done in the emergency room, but children might require general anesthesia because working near the eyes with sharp instruments can be frightening to the child and could pose a risk to the eye if the child moves suddenly. Additionally, pediatric canalicular repairs in the minor procedure room tend to have a higher rate of postoperative epiphora compared to those repaired in the operating room.1
Studies show that only 1% to 5% of patients with dog bites have coexistent facial fractures,1,4 so CT imaging is not recommended unless there is a high suspicion for a foreign body or fracture based on presentation. This is to minimize the risk of radiation on the developing child.
First use copious irrigation to wash the eye and remove any material that might contaminate the wound.
Superficial skin injuries of the lid that do not involve the margin can be sutured with interrupted or running 6‑0 fast gut or 7‑0 nylon or Prolene. To avoid the need for suture removal or if the patient has any suspicion for loss to follow-up, absorbable sutures can be used.
If the margin is affected, then it is very important to have accurate tarsal approximation to ensure good repair. With 6‑0 silk, place 2 or 3 vertical mattress sutures on the lid margin anterior to posterior at the lash line, gray line, and meibomian glands. After placing the suture, wait to tie it and leave the ends loose. Then, with 6-0 vicryl, place partial-thickness interrupted sutures to approximate the tarsus. Be careful to not pass too deeply into the palpebral conjunctiva because this can cause irritation after repair. Then tie the margin sutures and tarsal sutures, leaving long tails on the margin sutures so they can be anchored to the skin sutures. Next, close the pretarsal skin with either interrupted or running sutures as above, anchoring the margin suture tail. The margin suture should result in some degree of eversion of the wound edges.
Do not repair septum lesions, and take care when repairing levator or aponeurosis lesions, because accidentally suturing into the orbital septum can lead to postoperative lagophthalmos.
As mentioned previously, the most common cause of canalicular lacerations in children is dog bites. In a study of 137 patients by Murchison et al., the causes in older children were more likely to be sports injuries or altercations with other children.1 These lesions occur when the eyelid is either directly hit or indirectly damaged by horizontal traction, which subsequently avulses the lid at its weak points where there is no tarsal support at either the medial or lateral canthus. Diagnostic probing or irrigation might be needed to confirm a canalicular laceration. Lindberg and Moore5 show that even one nonfunctioning canaliculus can lead to epiphora in 50% of patients, therefore it is recommended that every lesion be repaired. Primary repair is more successful and should be performed within 48 hours.
Using a stent prevents postoperative stricture of the canaliculus and helps to oppose the two edges of the canalicular ducts; only the tissue around it requires suturing. Studies have shown that both monocanalicular and bicanalicular stents are effective in adults,6,7 and the pediatric cohort by Murchison and colleagues appears to show the same.1
Lastly, give prophylactic antibiotics and follow tetanus and rabies protocols when indicated. The most common bacterium in dog bites is Pasteurella species, but also include coverage for Staphylococcus, Streptococcus, and anaerobes. A beta-lactam antibiotic with a beta-lactamase inhibitor such as ampicillin-sulbactam works well.8 The stent can be removed after 3 months.
Orbital Fractures
The most common causes of orbital fractures in the pediatric age group are motor-vehicle accidents, sports, and falls, with falls being the most common in children younger than 5 years and sports injuries in children older than 5 years.1–15 Changes in the skeletal and facial architecture as a child develops lend to certain fractures being more or less common. In infancy, the larger brow protects the face, then as the child grows, the midface and mandible become more prominent and are more likely to become injured.7,15–18 This renders younger patients more likely to sustain orbital rim fractures, whereas older children and adolescents are more likely to have medial, lateral, and floor factors. Studies show that the age where likelihood for these fractures switches is about 7 years.8,19
The general approach to examining a child with a known or suspected history of facial trauma includes assessment of visual acuity, extraocular motility and forced ductions, as well as a thorough slit-lamp exam including any signs of corneal trauma, hyphema, lens dislocation, vitreous detachment, or open globe.20
If any abnormal exam findings are revealed or there is a known or suspected history of trauma, further workup with imaging is recommended. Additional indications include any deformity, crepitance, or stepoff on palpation, severe pain, proptosis, or enophthalmos, widened intercanthal distance, bradycardia as manifested by the oculocardiac reflex, and the inability to perform a detailed physical examination.20–23 CT is the test of choice because it is the best at evaluating bony structures, however, it is not so good for evaluation of soft tissue and has been shown to significantly underestimate entrapment of orbital contents.22,24,25
As mentioned, children and adolescents are more likely to sustain lateral wall, medial wall, and floor fractures, medial wall and floor fractures carrying the highest risk for entrapment. These trapdoor fractures are acknowledged to be more common in children than in adults and occur when the bony fragment, acting as a swinging door, pops open at the moment of blunt injury and subsequently swings closed again, entrapping orbital contents or extraocular muscles. The classic presenting symptoms of a trapdoor fracture include nausea and vomiting. It has been demonstrated that these symptoms carry a positive predictive value of 83.3% for inferior rectus entrapment.2 In addition, the patient might have diplopia or limited extraocular motility, forced ductions, and the well-known "oculocardiac reflex" causing significant bradycardia and indicating immediate surgical intervention.23,26,27 Another classic presentation is the "white-eyed blowout" in which the child has very minimal swelling of soft tissues, but poor extraocular motility and negative findings on imaging.22
The need for surgical intervention with orbital fractures depends on both clinical and radiological findings. Trapdoor fractures always require surgical repair. The proposed timing for surgery is anywhere within the first 24–48 hours because this has been shown to have the best long-term outcomes and extraocular motility recovery.1,20,23,24,28–32 For nonentrapped fractures, indications to intervene include
- enophthalmos (> 0.2 mm)
- nonresolving diplopia or intraorbital fragments causing diplopia
- fractures involving greater than 50% of the orbital floor
- need for intraorbital volume expansion
- globe malposition
- no clinical improvement over a few weeks8,22,23,29,33,34
The timing for repair of nonentrapped fractures is not well established. Regarding orbital roof fractures, the need for repair is much less common19 and indications for repair include fractures causing extraocular dysmotility or significant deformity of the superior orbital rim.8
The incidence of ophthalmic injuries from orbital trauma is fewer in children than in adults.16,34 Neurological injuries are more common complications and more often associated with orbital roof fractures.5,19,35–37 If fractures are found beyond the orbit, have high suspicion for neurological injury because these fractures carry a 7–8 fold increased risk compared to isolated orbital fractures.8,36
Retrobulbar Hemorrhage
One complication of blunt orbital trauma that deserves rapid evaluation and intervention is retrobulbar hemorrhage. There are two types, intrabulbar and subperiosteal, with intrabulbar being more common overall.38 With the orbital septum limiting anterior displacement of the globe, pressure builds behind the eye. This can rapidly lead to vision loss from compression of optic-nerve vasculature, direct optic neuropathy, and increased intraocular pressure leading to central retinal artery occlusion or retinal vasculature ischemia.39 Have high suspicion for retrobulbar hemorrhage in anyone with blunt trauma and associated chemosis, proptosis, pain, ophthalmoplegia, a hard eye, APD, or abnormalities on fundoscopy such as a pale disc or cherry red spot. CT and MRI can be used to evaluate the orbit and soft tissues, but do not delay management because there can be rapid vision loss within 90 minutes.
Treatment aims at quickly reducing orbital and intraocular pressure with both medical and surgical management. This is primarily done through a lateral canthotomy and cantholysis. After injecting local anesthetic with epinephrine, clip a hemostat on the skin at the lateral canthus for 1–2 minutes to provide hemostasis. Using scissors directed away from the globe, make an incision that extends to the lateral orbital rim. With retraction of the inferior lid and, again, scissors aimed away from the globe, dissect inferiorly to cut the lateral crus of the lateral canthal tendon. If increased pressure in the eye does not resolve, the super crus can be cut as well. Adjunctive medical management, including acetazolamide and 20% mannitol to relieve pressure as well as IV hydrocortisone,40 can be used, however, this should not delay surgical intervention.
Less frequently, a subperiosteal hematoma forms after a traumatic event. They are more commonly seen in children than adults because the periosteum is more loosely adherent to underlying bone and can more readily detach.41 Still, they represent only less than 1% of space occupying lesions in the orbit of children.42 In Yacizi et al., 23 cases of traumatic subperiosteal hematomas in children were reviewed, noting that 48% occurred from direct impact and 92% were located in the superior orbit. Decreased vision was found in 62% of patients on presentation, and 74% of these were treated with surgical drainage or needle aspiration.43 It is important to note, however, that any concern for a rapidly expanding, space-occupying lesion in the orbit with subsequent compartment syndrome should be managed with immediate decompression through lateral canthotomy with or without cantholysis.
Orbital Foreign Bodies
As with retrobulbar hemorrhage, always keep intraorbital foreign body on the differential of a child with trauma, no matter how trivial the event. Severe complications can occur, and children and adolescents are often poor historians, so it is important to evaluate for foreign bodies in any child with a history of eyelid or orbital trauma. Alternatively, it is important to inquire as to a history of trauma in any child with an orbital infection or inflammation without a known cause. Symptoms can lie anywhere on a large spectrum from completely asymptomatic to swelling, pain, or visual disturbances such as diplopia.44
Foreign bodies can be classified into inorganic or organic. Although metal or nonmetal inorganic bodies are more likely to cause direct trauma to the globe or orbital structures, organic foreign bodies often are more inflammatory and pose a high risk for serious orbital infections. CT (Figures 1–3) is the initial diagnostic test of choice, but has been shown to miss objects that are either very small or composed of certain organic material such as wood.45 Alternatively, MRI can be more sensitive for organic materials, but do not use it if there is any concern for a ferromagnetic object.
The treatment of intraorbital foreign bodies depends on a variety of factors. Fulcher et al. reviewed 40 cases and describe an algorithm for approach to treatment.46 All organic foreign bodies should be removed surgically. If the body is nonorganic, removal depends on location in the orbit, risk for surgical removal, and whether the patient is experiencing complications such as inflammation, restricted motility, or optic-nerve compression. If the body is located posterior and the patient does not have complications, surgery is not recommended. If the body is anterior and without complications, discuss with the parents to determine their preference. Collaborating with other specialists, specifically infectious disease specialists, in regard to antibiotic treatment is recommended. Use of broad-spectrum antibiotics with or without anaerobic and antifungal coverage is recommended, as is keeping the patient's tetanus vaccination up to date.46

Figure 1. Axial view of CT scan of orbit with foreign body (pencil).
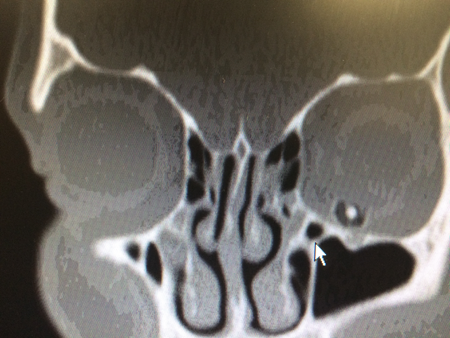
Figure 2. Coronal view of same patient: foreign body between eye and orbital floor.
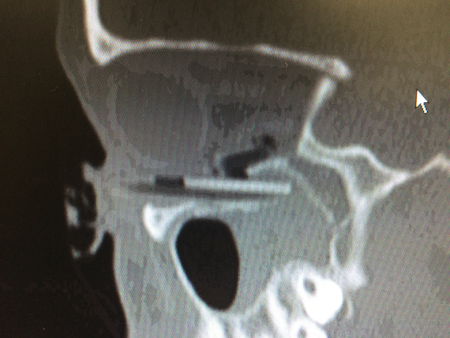
Figure 3. Sagittal view of orbit with foreign body (pencil).
Extraocular-Muscles Trauma
Direct muscle injury is uncommon. If ophthalmoplegia cannot be explained by adnexal or orbital injury, a central origin should be ruled out. Severe eyelid edema, orbital hemorrhage, or poor patient cooperation makes ocular motility examination impossible.
Optic-Nerve Trauma
Traumatic optic neuropathy (TON) occurs after head or orbital trauma.47,48 TON is found in 0.5–2% of patients with closed-head trauma. Bilateral optic-nerve involvement occurs in 5% of cases. Central vision can be severely affected, with 50% presenting visual acuities of light perception or worse. The most common causes of TON in children are falls, motor vehicle accidents, and sport injuries.
The optic nerve can be injured anywhere along its course, but most commonly at the intracanalicular and intracranial portion. It has been categorized as posterior or anterior (anterior to the entrance of the central retinal artery into the optic nerve). Direct optic-nerve injuries are a consequence of penetrating trauma such as orbital fractures, whereas indirect injuries arise when the impact to the skull is transmitted to the optic nerve.
Orbital hemorrhage and edema can lead to an orbital compartment syndrome, compromising circulation to the optic nerve. If the primary injury is transection or infarction, the result will be permanent visual loss. On the other hand, if compression in the optic canal is the consequence of hemorrhage and edema, medical and surgical interventions are indicated.
Traumatic optic neuropathy diagnosis is made with the clinical history and ophthalmological findings. The diagnosis is suspected in some cases by a new afferent pupillary defect in a traumatized eye without other ophthalmic lesions. Vision prognosis can be related to the initial visual acuities.
Vision assessment can be challenging when the patient's mental status is impaired due to trauma. In such cases, visual evoked potentials can be helpful. High-resolution computed tomography (CT) is the diagnostic procedure of choice. Bony fractures are better seen with CD than with magnetic resonance imaging (MRI).
The optic disk can look normal in the early stages after trauma. Papilledema and retinal hemorrhages can be found with injuries anterior to the entry point of the central retinal vessels. In optic nerve avulsion, the optic disk is missing and a hemorrhagic ring is present. If orbital hemorrhage compromises optic nerve circulation, perform lateral canthotomy and cantholysis immediately.
Management of TON remains controversial.49 Observation, high-dose steroids, and surgical decompression have been advocated, but there are no randomized clinical trials to support any of those options. In case of an optic nerve sheath hematoma, urgent decompression with sheath fenestration is indicated.
References
- Murchison AP, Bilyk JR. Pediatric canalicular lacerations: epidemiology and variables affecting repair success. Journal of pediatric ophthalmology and strabismus 2014;51:242-248.
- Savar A, Kirszrot J, Rubin PA. Canalicular involvement in dog bite related eyelid lacerations. Ophthalmic plastic and reconstructive surgery 2008;24:296-298.
- Slonim CB. Dog bite-induced canalicular lacerations: a review of 17 cases. Ophthalmic plastic and reconstructive surgery 1996;12:218-222.
- Wei LA, Chen HH, Hink EM, Durairaj VD. Pediatric facial fractures from dog bites. Ophthalmic plastic and reconstructive surgery 2013;29:179-182.
- Linberg JV, Moore CA. Symptoms of canalicular obstruction. Ophthalmology 1988;95:1077-1079.
- Lee H, Chi M, Park M, Baek S. Effectiveness of canalicular laceration repair using monocanalicular intubation with Monoka tubes. Acta ophthalmologica 2009;87:793-796.
- Leibovitch I, Kakizaki H, Prabhakaran V, Selva D. Canalicular lacerations: repair with the Mini-Monoka(R) monocanalicular intubation stent. Ophthalmic surgery, lasers & imaging : the official journal of the International Society for Imaging in the Eye 2010;41:472-477.
- Talan DA, Citron DM, Abrahamian FM, Moran GJ, Goldstein EJ. Bacteriologic analysis of infected dog and cat bites. Emergency Medicine Animal Bite Infection Study Group. The New England journal of medicine 1999;340:85-92.
- Chandler DB, Rubin PA. Developments in the understanding and management of pediatric orbital fractures. International ophthalmology clinics 2001;41:87-104.
- Cohen SM, Garrett CG. Pediatric orbital floor fractures: nausea/vomiting as signs of entrapment. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 2003;129:43-47.
- Eggensperger Wymann NM, Holzle A, Zachariou Z, Iizuka T. Pediatric craniofacial trauma. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 2008;66:58-64.
- Ferreira PC, Amarante JM, Silva PN, et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plastic and reconstructive surgery 2005;115:1500-1508.
- Fulcher TP, Sullivan TJ. Orbital roof fractures: management of ophthalmic complications. Ophthalmic plastic and reconstructive surgery 2003;19:359-363.
- Gassner R, Tuli T, Hachl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 2004;62:399-407.
- Hatef DA, Cole PD, Hollier LH, Jr. Contemporary management of pediatric facial trauma. Current opinion in otolaryngology & head and neck surgery 2009;17:308-314.
- Hink EM, Wei LA, Durairaj VD. Clinical features and treatment of pediatric orbit fractures. Ophthalmic plastic and reconstructive surgery 2014;30:124-131.
- Holland AJ, Broome C, Steinberg A, Cass DT. Facial fractures in children. Pediatric emergency care 2001;17:157-160.
- Imahara SD, Hopper RA, Wang J, Rivara FP, Klein MB. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. Journal of the American College of Surgeons 2008;207:710-716.
- Li Z, Li ZB. Characteristic changes of pediatric maxillofacial fractures in China during the past 20 years. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 2008;66:2239-2242.
- Losee JE, Afifi A, Jiang S, et al. Pediatric orbital fractures: classification, management, and early follow-up. Plastic and reconstructive surgery 2008;122:886-897.
- Messinger A, Radkowski MA, Greenwald MJ, Pensler JM. Orbital roof fractures in the pediatric population. Plastic and reconstructive surgery 1989;84:213-216; discussion 217-218.
- Nowinski D, Di Rocco F, Roujeau T, Meyer P, Renier D, Arnaud E. Complex pediatric orbital fractures combined with traumatic brain injury: treatment and follow-up. The Journal of craniofacial surgery 2010;21:1054-1059.
- Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: recent advances in prevention, diagnosis and management. International journal of oral and maxillofacial surgery 2006;35:2-13.
- Alcala-Galiano A, Arribas-Garcia IJ, Martin-Perez MA, Romance A, Montalvo-Moreno JJ, Juncos JM. Pediatric facial fractures: children are not just small adults. Radiographics : a review publication of the Radiological Society of North America, Inc 2008;28:441-461; quiz 618.
- Koltai PJ, Rabkin D. Management of facial trauma in children. Pediatric clinics of North America 1996;43:1253-1275.
- Meier JD, Tollefson TT. Pediatric facial trauma. Current opinion in otolaryngology & head and neck surgery 2008;16:555-561.
- Koltai PJ, Amjad I, Meyer D, Feustel PJ. Orbital fractures in children. Archives of otolaryngology--head & neck surgery 1995;121:1375-1379.
- Wei LA, Durairaj VD. Pediatric orbital floor fractures. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus / American Association for Pediatric Ophthalmology and Strabismus 2011;15:173-180.
- Chapman VM, Fenton LZ, Gao D, Strain JD. Facial fractures in children: unique patterns of injury observed by computed tomography. Journal of computer assisted tomography 2009;33:70-72.
- Jordan DR, Allen LH, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthalmic plastic and reconstructive surgery 1998;14:379-390.
- Sires BS, Stanley RB, Jr., Levine LM. Oculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repair. Archives of ophthalmology 1998;116:955-956.
- Criden MR, Ellis FJ. Linear nondisplaced orbital fractures with muscle entrapment. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus / American Association for Pediatric Ophthalmology and Strabismus 2007;11:142-147.
- Parbhu KC, Galler KE, Li C, Mawn LA. Underestimation of soft tissue entrapment by computed tomography in orbital floor fractures in the pediatric population. Ophthalmology 2008;115:1620-1625.
- Cobb A, Murthy R, Manisali M, Uddin J, Toma A. Oculovagal reflex in paediatric orbital floor fractures mimicking head injury. Emergency medicine journal : EMJ 2009;26:351-353.
- Kim J, Lee H, Chi M, Park M, Lee J, Baek S. Endoscope-assisted repair of pediatric trapdoor fractures of the orbital floor: characterization and management. The Journal of craniofacial surgery 2010;21:101-105.
- Bansagi ZC, Meyer DR. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology 2000;107:829-836.
- Carroll SC, Ng SG. Outcomes of orbital blowout fracture surgery in children and adolescents. The British journal of ophthalmology 2010;94:736-739.
- Grant JH, 3rd, Patrinely JR, Weiss AH, Kierney PC, Gruss JS. Trapdoor fracture of the orbit in a pediatric population. Plastic and reconstructive surgery 2002;109:482-489; discussion 490-485.
- McInnes AW, Burnstine MA. White-eyed medial wall orbital blowout fracture. Ophthalmic plastic and reconstructive surgery 2010;26:44-46.
- Yang JW, Woo JE, An JH. Surgical outcomes of orbital trapdoor fracture in children and adolescents. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery 2015;43:444-447.
- Burnstine MA. Clinical recommendations for repair of isolated orbital floor fractures: an evidence-based analysis. Ophthalmology 2002;109:1207-1210; discussion 1210-1201; quiz 1212-1203.
- Holt GR, Holt JE. Incidence of eye injuries in facial fractures: an analysis of 727 cases. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 1983;91:276-279.
- Donahue DJ, Smith K, Church E, Chadduck WM. Intracranial neurological injuries associated with orbital fracture. Pediatric neurosurgery 1997;26:261-268.
- Greenwald MJ, Boston D, Pensler JM, Radkowski MA. Orbital roof fractures in childhood. Ophthalmology 1989;96:491-496; discussion 496-497.
- Whatley WS, Allison DW, Chandra RK, Thompson JW, Boop FA. Frontal sinus fractures in children. The Laryngoscope 2005;115:1741-1745.
- Wolter JR, Leenhouts JA, Coulthard SW. Clinical picture and management of subperiosteal hematoma of the orbit. Journal of pediatric ophthalmology 1976;13:136-138.
- Dolman PJ, Glazer LC, Harris GJ, Beatty RL, Massaro BM. Mechanisms of visual loss in severe proptosis. Ophthalmic plastic and reconstructive surgery 1991;7:256-260.
- Ord RA. Post-operative retrobulbar haemorrhage and blindness complicating trauma surgery. The British journal of oral surgery 1981;19:202-207.
- Bourdon EL, Riffaud L, Godey B, Morandi X. [Subperiosteal hematoma of the orbit associated with a frontal extradural hematoma]. Journal francais d'ophtalmologie 1999;22:659-661.
- Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008.
- Yazici B, Gonen T. Posttraumatic subperiosteal hematomas of the orbit in children. Ophthalmic plastic and reconstructive surgery 2011;27:33-37.
- Al-Mujaini A, Al-Senawi R, Ganesh A, Al-Zuhaibi S, Al-Dhuhli H. Intraorbital foreign body: clinical presentation, radiological appearance and management. Sultan Qaboos University medical journal 2008;8:69-74.
- Green BF, Kraft SP, Carter KD, Buncic JR, Nerad JA, Armstrong D. Intraorbital wood. Detection by magnetic resonance imaging. Ophthalmology 1990;97:608-611.
- Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology 2002;109:494-500.
- Goldenberg-Cohen N1, Miller NR, Repka MX. Traumatic optic neuropathy in children and adolescents. J AAPOS. 2004;8(1):20-7
- Ford RL, Lee V, Xing W, Bunce C. A 2-year prospective surveillance of pediatric traumatic optic neuropathy in the United Kingdom.JAAPOS. 2012; 16(5): 413-7
- Kumaran AM, Sundar G, Chye LT. Traumatic optic neuropathy : a review. Craniomaxillofac Trauma Reconstr. 2015;8(1):31-41