Download PDF
Harper Herbert,* a healthy 20-year-old woman, had just returned to college from her winter break when she started noticing progressive blurry vision in both eyes. She had recently undergone LASIK in both eyes while vacationing back home in California. While there, Ms. Herbert showed up for her postoperative visits, followed instructions, and took all necessary precautions. She even initially obtained the perfect vision that she had hoped for after LASIK. Now, she felt like she was looking through a fog.
We Get a Look
Ms. Herbert presented to our clinic two weeks after she had undergone LASIK. She started noticing problems about two days before she saw us, and she was frustrated. She told us that she hadn’t experienced any pain, photosensitivity, trauma, or foreign body sensation. The day before arriving at our clinic for evaluation, she had seen a local optometrist who started her on Pred Forte (prednisolone acetate 1%) every hour in both eyes.
On exam, her uncorrected visual acuity (VA) was 20/50 in her right eye and 20/100 in her left. With the use of a pinhole, this improved to 20/30+2 and 20/20, respectively. We used a Tono-Pen (Reichert) to measure her IOP, which was 13 mm Hg in her right eye and 16 mm Hg in her left. There were no visual field or afferent pupillary defects, and her ocular motility was intact in both eyes.
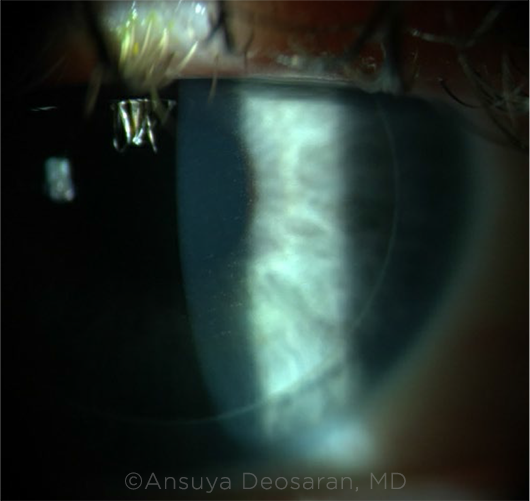
Her slit-lamp exam showed a slight diffuse haze to both corneas with a fine granularity to the flap interface and anterior stroma in both eyes. The conjunctivae were white and quiet, and there were no cells in the anterior chamber of either eye.
On the dilated fundus exam, there was a normal optic nerve, macula, retinal vessels, and peripheral retina in both eyes.
 |
|
WE GET A LOOK. We noted a fine granularity at the flap interface of both eyes.
|
Initial Misdiagnosis
Given the diffuse haze and granules in both eyes, we speculated that Ms. Herbert was presenting with a case of diffuse lamellar keratitis (DLK), though we realized that its typical time course is within the first postoperative week of LASIK.
We started her on intense steroids, which included difluprednate 0.05% hourly and prednisone 60 mg daily by mouth. The following day, her BCVA was 20/70 in her right eye and 20/50 in the left. She reported having nausea and headaches, but she assumed that this was because she was straining to see. Her IOP measured in the corneal periphery with a Tono-Pen was 23 mm Hg in her right eye and 32 mm Hg in the left. Her slit-lamp exam still showed anterior stromal haze with some granularity in both eyes. Now, we had to reconsider her diagnosis; was this DLK or was this pressure-induced stromal keratopathy (PISK)?
Making the Diagnosis
We decided to stop the prednisone, decrease the difluprednate regimen, and start IOP-lowering medications (topical brimonidine tartrate 0.2%, timolol 0.5%, and acetazolamide 500 mg). With this change, Ms. Herbert’s headaches and nausea resolved, but her pristine vision still had yet to return. We therefore instructed her to cease using all steroid medication and continue with the IOP-lowering medications as well as Muro-128 (sodium chloride) 5%. Subsequently, her VA dramatically improved and returned to 20/20 in both eyes three days later. Ms. Herbert’s drastic improvement off all steroids and transition to IOP-lowering medications confirmed the diagnosis of PISK.
Discussion
PISK is a rare but severe complication seen after LASIK. Following this surgery, a potential space between the LASIK flap and stromal bed is created by the microkeratome or laser.
It is theorized that elevated IOP causes fluid transudation across the endothelium and into that space.1,2 Steroids can cause elevated IOP, which can lead to this malfunction in fluid dynamics. An IOP response is seen in about 5%-30% of patients using steroids, which can be prescribed for a wide variety of conditions.3 Although a steroid-related rise in IOP typically takes two to six weeks, it has been documented to occur much sooner in some patients.3 Vision loss in patients with PISK is likely due to abrupt rise in IOP, edema of the flap, fluid in the interface, brief changes in the index of refraction, and microcracks in Bowman’s membrane.2
Presentation. Patients with PISK typically present with decreased vision about 10 to 14 days following surgery; however, these patients can present several months or even years afterward.1 As in this case, patients may present with symptoms of elevated IOP, such as headaches and nausea. It’s also worth noting that there may be an elevated IOP, but the space-occupying interface fluid can lead to an underestimated measurement. This is particularly true if the IOP measurement is based on a reading at the central cornea. For more accurate results, you can take IOP measurements with a Tono-Pen or Schiotz tonometer in the corneal periphery or use a dynamic contour tonometer.2,3 This presumably explains why our second set of IOP measurements, taken at the corneal periphery, were considerably higher than those we recorded when we first saw her.
Exam findings. On slit-lamp exam, patients may have a diffuse haze confined to the flap interface, typically without granules; yet it is possible to see granularity, as in Ms. Herbert’s case. No anterior chamber reaction is seen in PISK. Sometimes, a distinct fluid cleft between the flap and stroma may be visible; however, this is not always found on exam.4 An anterior segment OCT can be used to aid with diagnosis and show the fluid cleft if present.2 Confocal microscopy may be of less clinical value but has shown that PISK lacks mononuclear cells and granulocytes.3
Complications and management. PISK should always be considered in any DLK-like presentation beyond one week of LASIK and in patients who fail to respond to steroids. The main treatment for PISK is to stop all steroids and treat the IOP. Dorzolamide should be avoided as it can disturb the function of the endothelial pumps and theoretically worsen PISK.5 These patients require close follow-up to ensure that fluid and haze disappear and IOP normalizes.
There is also a risk of epithelial in-growth. The fluid cleft may lift the edges of the LASIK flap, allowing epithelial cells to access and grow into the flap-stromal interface. Due to elevated IOP, glaucoma with visual field defects, central vision loss, and glaucomatous optic neuropathy have also been reported.4 Therefore, consider PISK in post-LASIK patients who are presenting with glaucomatous exam findings. Delayed onset of PISK has been reported years after surgery in patients started on steroids for uveitis.1 PISK has also been reported following small-incision lenticule extraction (SMILE) procedures as there is a potential space for fluid to accumulate.5
Differential diagnosis. It is important to be able to distinguish PISK from DLK as treatment for the latter (steroids) is contraindicated for the former. DLK is a sterile inflammatory reaction that can present with visual complaints similar to those seen in PISK. DLK patients may show a hazy cornea confined to the flap interface and a classic granular appearance known as “sands of Sahara.”5 However, several features will aid in distinguishing DLK from PISK. First, DLK presents within the first post-op week (usually one to three days after surgery) and with a normal IOP. Conversely, PISK presents beyond one week postoperatively and has increased IOP. In addition, aggressive steroid drops are used to improve DLK; in contrast, it is the response to the steroids that causes PISK.4 Another misdiagnosis is post-LASIK infectious keratitis. Redness, photophobia, pain, and a more focal reaction can be clues to help distinguish this potential differential.
Prognosis. When identified and diagnosed early, PISK tends to be highly responsive to treatment, and patients are left with good visual outcomes.
___________________________
*Patient name is fictitious.
___________________________
1 Lee V et al. Cornea. 2012;31(1):87-89.
2 Cabral-Macias J et al. J Cataract Refract Surg. 2018;44(10):1284-1290.
3 Tourtas T et al. Cornea. 2011;30(8):920-923.
4 Davidson RS et al. J Glaucoma. 2003;12(1):23-26.
5 Moshirfar M et al. Cornea. 2020;39(2):254-257.
___________________________
The authors thank Nicholas Reyes, MS, for his assistance with this article. Mr. Reyes is a medical student who attended the University of Queensland–Ochsner Clinical School in New Orleans. Dr. Deosaran is a cornea fellow at Washington University School of Medicine in St. Louis. Dr. Shah is a cornea specialist at Ochsner Medical Center in New Orleans. Financial disclosures: None.
MORNING ROUNDS: 2021 IN REVIEW
Tackle this year’s medical mysteries:
Who Dimmed the Lights? Headache, Eye Pain, and Fading Vision. After five days of dimming vision, the 24-year-old couldn’t see out of her right eye, and now her left eye was getting worse, too (January 2021).
A Man With a Sleepy Appearance. The 57-year-old was increasingly being told that he had a “sleepy” appearance—and was also having more difficulty in driving, reading, and using the computer (February 2021).
Weighed Down by an Anchor. Several doctors had told the 78-year-old that his vision loss was due to “a blood clot in the eye” (March 2021).
The Lively 4-Year-Old and the Growing Lesion. Her parents had noticed redness in the corner of her eye for about a year (April 2021).
A Mysterious Amelanotic Fundus Mass. The 38-year-old was referred to us because of a freckle at the back of her left eye. Apart from some eye strain when using the computer, she hadn’t noticed any vision problems (May 2021).
Not Your Typical Headlight in the Fog. The 11-year-old had experienced blurry vision for two months before she was referred to us for retinal inflammation. What’s your diagnosis? Web Extra: OCT images showing improvement in the chorioretinal lesion three weeks after the initial presentation and complete resolution of the subretinal fluid following anti-VEGF therapy (July 2021).
A Case of Blurred Vision With Ocular Pain. The 24-year-old had never had a headache like this before. After a week of blurry vision, with floaters and flashes, she woke up with significant ocular pain (October 2021).
A Nail Gun, a Ruptured Globe—and a Surprise. His ruptured globe was repaired, but the eye became increasingly inflamed (November 2021).
|