By Miguel Paciuc, MD; Jose Dalma-Weiszhausz, MD; Ryan Phan, MD; David Smits, MD; Raul Velez-Montoya MD
According to the Birmingham Eye Injury classification (BETT),1 open-globe injuries involve the total thickness of the eye wall: cornea and/or sclera. They range from a small, penetrating, self-sealing pin prick to globe rupture with total disorganization and prolapse of intraocular contents. Open-globe injuries compose about 10% of all eye injuries, but the numbers vary according to the series. In one study involving injuries that required hospitalization, 28% were open-globe injuries and 4% involved an intraocular foreign body (IOFB).2 Most injuries are caused by various sharp objects (22%).
Penetrating wounds are usually caused by sharp objects that deliver enough energy in a small area that it allows the object to enter the eye wall. When the causing object enters and remains inside the eye, it is considered an intraocular foreign body. When it carries enough energy to exit the eye wall, causing entry and exit wounds, it is called a perforating injury. Ruptures occur when the incident object carries enough energy to deform the eye and increase IOP enough to make the wall explode, often extruding intraocular tissue. The mechanism of these injuries is very different and so are the resulting associated damages and consequences.
Corneal and Scleral Wounds
Trauma caused by blunt objects is a major cause of corneal/scleral wounds; 30% of serious ocular injuries involve purely the sclera, whereas 10% involve the cornea and sclera. Most of these injuries are suffered by males in a ratio of almost 5:1. The majority of these injuries happen at home.3 The presence of subconjunctival hemorrhage, chemosis, or even a small break in the eyelid skin can be the only surface sign of scleral perforation by a sharp object. Pupil distortion can be the most apparent sign of a small corneal or limbal perforation.4 Clinical findings that suggest scleral ruptures include visual acuity of light perception or no light perception, chemosis, 360‑degree subconjunctival hemorrhage, hyphema, IOP < 10 mm Hg, a peaked pupil, and relative displacement of the lens-iris diaphragm.1
When faced with a history of a penetrating cornea/scleral trauma, the presence of intraocular foreign bodies must be ruled out. Consider CT of the orbits if an intraocular foreign body is suspected. Goals of management include restoration of the integrity of the globe, avoidance of further injury to ocular tissues, and prevention of corneal scarring and astigmatism.
Corneoscleral lacerations in children are repaired according to the same principles as for adults. Small conjunctival lacerations are often self-sealing. Superficial and lamellar corneal wounds can be managed with topical antibiotics and patching. A bandage contact lens might be needed to maintain a flap in place while healing. Small wounds can be managed conservatively, but large wounds usually require surgical repair by primary closure or patch grafting. Because corneal lacerations in children heal relatively quickly, sutures can be removed earlier.2
As long as vision is not affected, deep, inert foreign bodies can be left in the cornea. If a decision for removal is made, do so under the surgical microscope, taking care not to push the foreign body into the anterior chamber. Small, self-sealing, penetrating wounds are best managed with topical antibiotics and patching for a short time. Larger wounds might need tissue glue, but most will require suturing. The closure of these wounds should be watertight and cause as little distortion as possible of the normal corneal dome shape. This is best achieved by placing full-thickness, interrupted, 10‑0 nylon sutures starting with points that are easy to align (limbus, wound angles, etc.). Long, tighter sutures in the periphery of the cornea and shorter, looser sutures towards the center tend to preserve a more physiologic corneal shape. Make sure the wound is free of all foreign material and tissue.
Replace an extruded iris into the anterior chamber unless it is obviously necrotic or contaminated. This is best achieved through a limbal paracentesis, pulling the iris in rather than pushing through the wound. Intracameral viscoelastics are priceless in dealing with extruded tissues. Thoroughly cleanse entrapped lens material and vitreous to leave the wound edges free.
Approach corneoscleral and scleral lacerations by first closing the corneal or distal portion and then examining the extent of the scleral portion by carefully removing the conjunctiva and Tenon's capsule, closing the wound as it is uncovered. It is often necessary to disinsert one of the extraocular muscles to visualize and repair a wound that extends posteriorly.3 Take care not to distort the eye too much in trying to reach the posterior extent of a wound. Sometimes it is better to let Tenon's capsule spontaneously seal this portion of the injury.
Once the eye is hermetically sealed, restore the IOP by injecting balanced salt solution, preferably through an area where the needle-tip can be visualized, which might not always be possible. At this point, decide on the need and timing for further surgery. If a vitrectomy seems necessary, visualization is adequate, and human and material resources are available, continue the procedure at this time. If visualization is impaired due to corneal edema, the surgery can be postponed a few days.
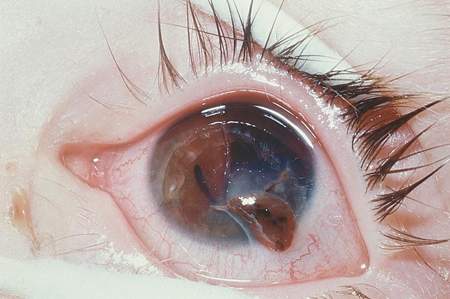
Figure 1. Open-globe injury: corneal lesion with iris prolapse.
Intraocular Foreign Bodies
Always suspect an intraocular foreign body (IOFB) in eye trauma regardless of how trivial or benign its initial appearance is. This is especially true in children, for whom the clinical history can be incomplete or absent. Children are often victims of trauma as bystanders or in play and might not be aware of the trauma until vision becomes compromised. Children are also afraid of reprimands, so they might hide critical data regarding the circumstances of the injury.
If the child behavior allows it and the eye wall injury is self-sealing, examine the globe as comprehensively as possible. The best way to detect an IOFB is by direct visualization at the slit-lamp or with the indirect ophthalmoscope.4 Media opacities often preclude such an exam.
CT scan is probably the best way of determining the presence of an IOFB in the posterior segment when visualization is reduced. Helical techniques with 3 mm collimation and overlapping cuts will detect most IOFBs with minimal radiation exposure and time. Sedation might be required to obtain good-quality images in small children.
B-scan ultrasound can offer certain advantages in determining the state of intraocular structures such as vitreous hemorrhage, retinal detachment, and choroidal hemorrhage.
If the eye-wall wound is large or unstable, repair it surgically before undertaking these diagnostic techniques. Transoperative ultrasonography can be done sterilely at the time of wound repair and surgery can continue as needed.
The threat of endophthalmitis justifies the urgency of IOFB removal in high-risk cases, especially when dealing with contaminated, organic or toxic IOFBs. In cases of retained IOFBs, endophthalmitis is estimated to occur in 0%–10.7%.5 The risk of endophthalmitis and proliferative vitreoretinopathy both decrease if the IOFB is removed within the first 24 hours.6 Interestingly, this risk has not been found to be related with composition of the foreign body.5,6 Previous studies have identified that initial visual acuity is an important predictive factor of visual outcome in patients with retained IOFBs.7 Vision loss results from cornea scarring, cataract, endophthalmitis, retinal detachment and toxicity of ionized iron (Siderosis Bulbi) in the intraocular tissues.
Another important observation is that eyes with retained anterior segment foreign bodies do better than those with posterior foreign bodies. The same is true for smaller objects.8 The presence of an IOFB is often accompanied by other pathology, which must be addressed at the time of initial repair and IOFB removal.
Extrabulbar Tissue Prolapse
Tissue prolapse is usually visible on inspection unless the wound is posterior and underneath a congested, edematous conjunctiva or blood-stained Tenon's capsule. Echography or CT scan can demonstrate tissue prolapse, although this is rarely needed. Tissue prolapse can also occur during transportation or be due to poor patient instruction and lack of eye shielding. As soon as an open-globe injury is suspected, keep diagnostic manipulations to a minimum.9
Intraocular tissue extrusion often accompanies and complicates ocular trauma. Tissue prolapse is defined as extrusion of intraocular content outside its normal compartment. This can be intrabulbar, exemplified by the presence of vitreous in the anterior chamber, or extrabulbar, as seen with iris or vitreous exposed through a corneal wound. Tissue prolapse occurs in 70% of ocular ruptures. This extrabulbar tissue extrusion ensues when intraocular and external pressures try to equalize through an open wound: The larger the difference in pressures, the more violent the protrusion of tissue. This is why globe rupture has a higher risk and severity of tissue prolapse as opposed to a penetrating wound.
Entrapped tissues help seal the wound and maintain intraocular pressure. But if left in place they become fixed to wound edges with fibrin within a few hours and permanently by fibrosis within a few days. This prevents adequate wound healing, can produce hypotension through leakage or ciliary body dysfunction, keeps the way open for infection and epithelial ingrowth, and can lead to chronic inflammation, corneal edema, macular edema, and retinal detachment.
Reposition viable cellular structures (iris, ciliary body, choroid, and retina) even if they have been exposed for more than 24 hours. If the iris is contaminated or epithelialized, excise it if necessary, but conserve as much tissue as possible. Excision of uveal tissues can lead to severe bleeding, inflammation, and phthisis. Uveal tissue manipulation leads to severe inflammation that requires intense anti-inflammatory therapy. Excise vitreous and lens prolapse to leave the wound completely clean and free. If there is a question as to the identity of the exposed material, make every effort to replace it in the eye.
Perforating Injuries
Ocular injuries in children account for 20%–50%1–3 of all ocular injuries. Perforating eye injuries make up 21–24%4,5 of serious ocular trauma and are a significant cause of visual loss. It is estimated that they can be prevented in up to 90% of cases.6 There is a male predominance of 2–6:13,7 in children more than 3 years old, which could be explained by the types of activities in which boys engage. Source of trauma correlates with age group. Injury incidence caused by consumer products is stable in children aged 2–12 years, but increases after 12 years of age.8 Sports- and gun-related injuries increase at 17 years8,9 whereas desk-supplies injuries are higher in children aged 5 to 8 years.9 The most common source of injury in 2- to 4-year-olds is toys. Firearms were the cause of 19% of all penetrating injuries in a US series.10 A US study from 1982 found that 16% of sports-related eye injuries in children cause perforation1.1 Perforating injuries from motor vehicle accidents has decreased since seat-belt use was made compulsory.12
Injuries from compressed air powered guns like BB guns and paintball air guns have a high preponderance in the male population. Visual outcome from this type of injury is very poor.10 In a UK series, dart-related injuries were the most common mechanism of penetrating injury for children. Visual outcome from these types of injuries was poor but better than air-gun related injuries.12
Prevention is a main component in reducing the incidence of these injuries. Because more than half of injuries happen at home or during play,6 instruct caregivers in preparing a safe home environment for children, for example, purchasing round-cornered furniture, providing safer tools such as blunt-nosed scissors, and restricting dangerous household utensils.14
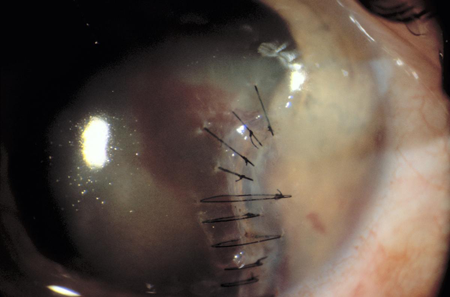
Figure 2. Repaired corneal injury.
References
- Nelson LB, Wilson TW, Jeffers JB. Eye injuries in childhood: demography, etiology, and prevention. Pediatrics. 1989;84(3):438-441.
- Jandeck C, Kellner U, Bornfeld N, Foerster MH. Open globe injuries in children. Graefes Arch Clin Exp Ophthalmol. 2000;238(5):420-426.
- Lindsey J, Bowes Hamill M. Chapter 15. Scleral and Corneoscleral Injuries from Ocular Trauma: Principles and Practice. Thieme 2011; 123-130
- Greven CM, Engelbrecht NE, Slusher MM, Nagy SS. Intraocular foreign bodies: Management, prognostic factors and visual outcomes. Ophthalmology 107 (3): 608-613
- Mieler WF, Ellis MK, Williams DF, Han DP. Retained intraocular foreign bodies and endophthalmitis. Ophthalmology 97: 1532-1538
- Brinton GS, Topping TM, Hyndiuk RA et al. Posttraumatic endophthalmitis. Arch Ophthalmol 102: 547-550
- Pieramici DJ, MacCumber MW, Humayun MU, et al. Open-globe injury. Update on types of injuries and visual results. Ophthalmology 103:1793-1803
- Woodcock M, Scott R, Huntbach J, Kirkby G. Mass and Shape as Factors in Intraocular Foreign Body Injuries. Ophthalmology. 2006. 113;12:2262-2269
- Dalma-Weiszhausz J. Chapter 16. Extrabulbar tissue prolapse from Ocular Trauma: Principles and Practice. Thieme 2011; 123-130.
- Punnonen E. Epidemiological and social aspects of perforating eye injuries. Acta Ophthalmol 1989;67:492–8
- Blomdahl S, Staffan N. Perforating eye injury in the Stockholm population. An epidemiological study. Acta Ophthalmol 1984;62:378–90
- Moreira CA, Debert-Ribeiro M, Belfort R. Epidemiological study of eye injuries in Brazilian children. Arch Ophthalmol 1988;106:781–4
- Brophy M, SA Sinclair, SG Hostetler, et al. Pediatric eye injury-related hospitalizations in the United States. Pediatrics 2006;117: 1263-1267
- Strahlman E, Elman M, Daub E, et al. Causes of pediatric eye injures. A population-based study. Arch Opthalmol 108:603-606
- Pizzarello LD. Ocular trauma:time for action. Opthalmic Epidemiol 1998. 5:115-116
- Rudd JC, Jaeger EA Freitag SK, et al. Traumatically ruptured globes in children. J Paediatr Ophthalmol Strabismus 1994;31:307–11.
- Alfaro DV, Chaudhry NA, Walkoner AF, et al. Penetrating eye injuries in young children. Retina 1994;14:201–5.
- Moren Cross J, Griffin R, Owsley C, et al. Pediatric eye injuries related to consumer products in the United States, 1997-2006. J AAPOS 12:626-628
- Shuttleworth GN, Galloway P, Sparrow JM. Ocular air gun injuries: a one-year surveillance study in the UK. Eye 23:1370-1376
- Luff AJ, Hodgkijns PR, Baxter RJ, et al. Aetiology of perforating eye injury. Arch Dis Child 1993;68:682–3.
- Cole MD, Clearkin L, Dabbs T, et al. The seat belt law and after. Br J Opthalmol 71:436-440
- Cole MD, Smerdon D. Perforating eye injuries caused by darts. Br J Opthalmol 72:511-514
- Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Survey of Opthalmology 59: 480