EPIDEMIOLOGY
Global Information
- Worldwide, diabetic retinopathy is the leading cause of blindness among working-aged adults.
- Global burden of diabetic retinopathy: 93 million people
- Proliferative diabetic retinopathy: 17 million
- Diabetic macular edema: 21 million
- Vision-threatening diabetic retinopathy: 28 million
- Prevalence of diabetic retinopathy is worldwide with only slight ethnic differences.
Region-Specific Information (Asia Pacific)
|
Table 1. Epidemiology Statistics for the Asian Region
|
|
Prevalence of diabetic retinopathy
|
23%
|
|
Prevalence of nonproliferative diabetic retinopathy
|
19.1%
|
|
Prevalence of proliferative diabetic retinopathy
|
2.8%
|
|
Prevalence of vision-threating diabetic retinopathy (in Singapore and Malaysia)
|
10%
|
|
Prevalence of diabetic retinopathy in type 2 diabetic patients (in Thailand)
|
31.4%
|
|
Prevalence of diabetic retinopathy in type 1 diabetic patients (in Thailand)
|
21.6%
|
DIFFERENTIAL DIAGNOSIS
PATHOPHYSIOLOGY/DEFINITION
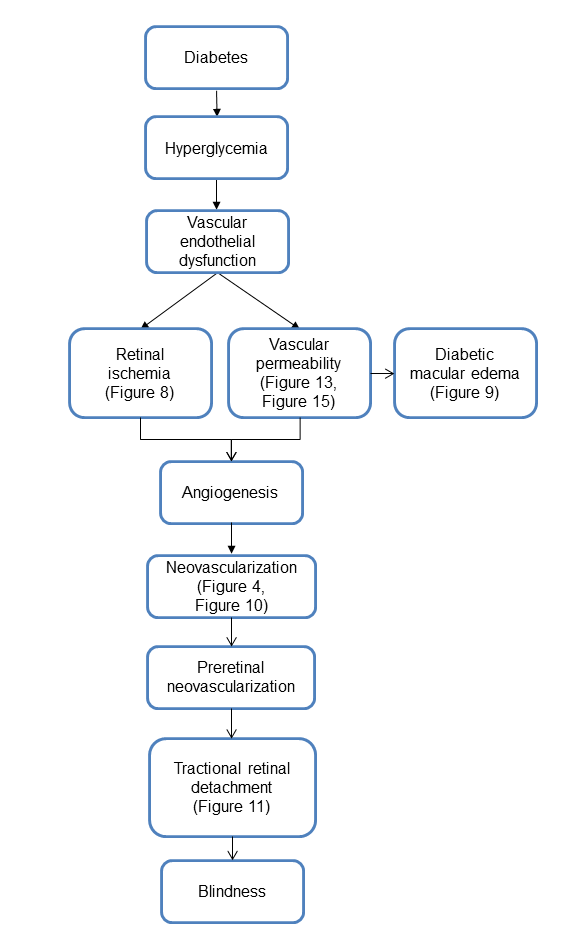
Chart 1. Pathophysiology. See Image Library for figures.
Risk Factors
- Blood glucose
- Duration of diabetes
- Blood pressure
- Blood lipids
- Renal impairment
- Pregnancy
SIGNS/SYMPTOMS
- Asymptomatic
- Decreased vision
- Floaters
- Metamorphopsia
- Symptoms of retinal detachment
- Examination findings consistent with pathophysiology (Chart 1)
MANAGEMENT
Classification
See Table 2.
|
Table 2. International Clinical Diabetic Retinopathy Disease Severity Scale
|
|
Proposed Disease
Severity Level
|
Findings Observable Upon Dilated Ophthalmoscopy
|
|
No apparent retinopathy
|
No abnormalities
|
|
Mild NPDR
|
Microaneurysms only (Figure 13)
|
|
Moderate NPDR
|
More than just microaneurysms but less severe NPDR
|
|
Severe NPDR
|
Any of the following and no signs of proliferative retinopathy:
- More than 20 intraretinal hemorrhages in each of four quadrants
- Definite venous beading in 2 or more quadrants (Figure 14)
- Prominent IRMA in 1 or more quadrants (Figure 15)
|
|
PDR
|
One of both of the following:
|
IRMA = intraretinal microvascular abnormalities; NPDR = nonproliferative diabetic retinopathy; PDR = proliferative diabetic retinopathy
Source: American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern® Guidelines. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008 (4th printing 2012). Available at: www.aao.org/ppp.
Treatment of Diabetic Macular Edema
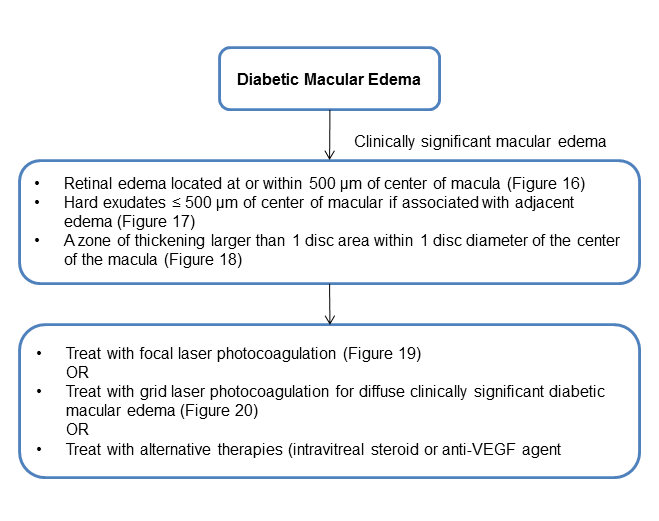
Chart 2. Treatment of diabetic macular edema. See Image Library for figures.
Management of Diabetic Retinopathy
See Table 3.
|
Table 3. Management Recommendations for Patients With Diabetes
|
|
Severity of Retinopathy
|
Presence of CSME
|
Follow-up (Months)
|
Panretinal Photocoagulation (Scatter) Laser
|
Fluorescein Angiography
|
Focal and/or Grid Laser
|
|
Normal or minimal NPDR
|
No
|
12
|
No
|
No
|
No
|
|
Mild to moderate NPDR
|
No
|
6–12
|
No
|
No
|
No
|
|
Yes
|
2–4
|
No
|
Usually
|
Usually
|
|
Severe NPDR
|
No
|
2–4
|
Sometimes
|
Rarely
|
No
|
|
Yes
|
2–4
|
Sometimes
|
Usually
|
Usually
|
|
Non–high-risk PDR
|
No
|
2–4
|
Sometimes
|
Rarely
|
No
|
|
Yes
|
2–4
|
Sometimes
|
Usually
|
Usually
|
|
High-risk PDR
|
No
|
2–4
|
Usually
|
Rarely
|
No
|
|
Yes
|
2–4
|
Usually
|
Usually
|
Usually
|
|
Inactive/
involuted PDR
|
No
|
6–12
|
No
|
No
|
Usually
|
|
Yes
|
2–4
|
No
|
Usually
|
Usually
|
CSME = clinically significant macular edema; NPDR = nonproliferative diabetic retinopathy; PDR = proliferative diabetic retinopathy
Source: American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern® Guidelines. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008 (4th printing 2012). Available at: www.aao.org/ppp.
CASE STUDY
This study describes the efficacy of anti-VEGF in promotion regression of retinal neovascularization.
History of Present Illness
A 38-year-old female was referred to the hospital for treatment of diabetic retinopathy.
Past Medical History
- Type II diabetes mellitus for 15 years
- Hypertension
Medications
Further Information
- Fasting blood sugar level ~180 mg%
- HbA1C at 7.3
Examination
- Visual acuity 20/25 RIGHT eye; 20/80 LEFT eye
- Intraocular pressure: 14 mm Hg BOTH eyes
- Slit-lamp examination: Unremarkable, NO iris neovascularization
- Fundus examination: Proliferative diabetic retinopathy with diabetic macular edema in both eyes with the LEFT eye worse than the RIGHT eye (Figure 26A)
Treatment
- Intravitreal injection of bevacizumab. One week after the treatment the patient’s fundus examination showed much improvement of the proliferative diabetic retinopathy (Figure 26B).
- The patient was treated with panretinal photocoagulation to promote further regression of retinal neovascularization and prevent worsening of the PDR.
IMAGE LIBRARY
Differential Diagnosis

Figure 1. Hypertensive retinopathy. Note the disc edema, macular exudates, intraretinal hemorrhage with nerve fiber layer infarct, and venous congestion.
(© 2013 American Academy of Ophthalmology.)
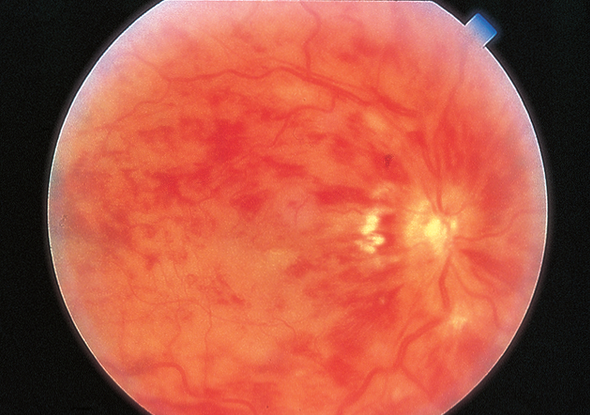
Figure 2. Central retinal vein occlusion (CRVO). CRVO in an eye with hand motions vision. The veins are dilated, and retinal hemorrhages are present. (© 2013 American Academy of Ophthalmology.)

Figure 3. Branch retinal vein occlusion. (© 2013 American Academy of Ophthalmology.)

Figure 4. Neovascularization of disc. (Reprinted from the Digital Reference of Ophthalmology, Retina and Vitreous, Retinal Vascular Disease, with permission from the Edward S. Harkness Eye Institute, Department of Ophthalmology of Columbia University.)

Figure 5. Radiation retinopathy. Image of an eye that has undergone plaque brachytherapy for treatment of choroidal melanoma. The melanoma can be seen nasally, obscuring part of the disc. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of Tara A. McCannel, MD, PhD.)

Figure 6. Sickle cell retinopathy, with peripheral neovascularization (“sea fan” neovascularization) with autoinfarction. (© 2013 American Academy of Ophthalmology.)
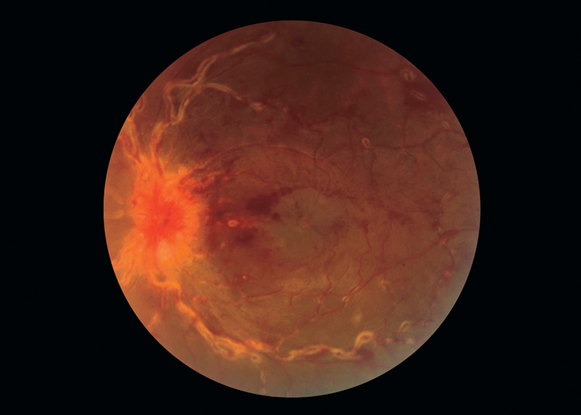
Figure 7. Sarcoidosis, with retinal vascular sheathing. (© 2013 American Academy of Ophthalmology.)
Pathophysiology/Definition
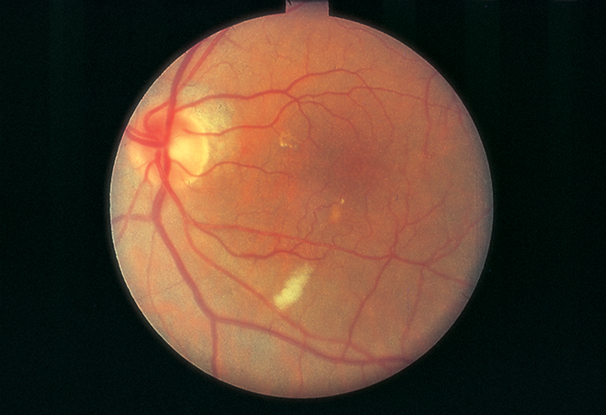
Figure 8. Cotton-wool spot (capillary retinal arteriole obstruction). (© 2013 American Academy of Ophthalmology.)
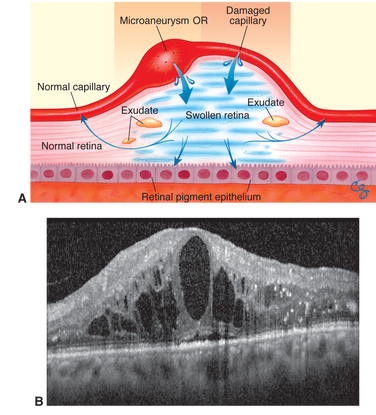
Figure 9. Diabetic macular edema. A.Mechanism of diabetic macular edema, demonstrating development of thickening from a breakdown of the blood–retinal barrier. B. Spectral-domain optical coherence tomogram of diabetic macular edema. Note the foveal detachment. (© 2013 American Academy of Ophthalmology.)

Figure 10. Retinal neovascularization. (Image courtesy of Kellogg Eye Center, University of Michigan.)
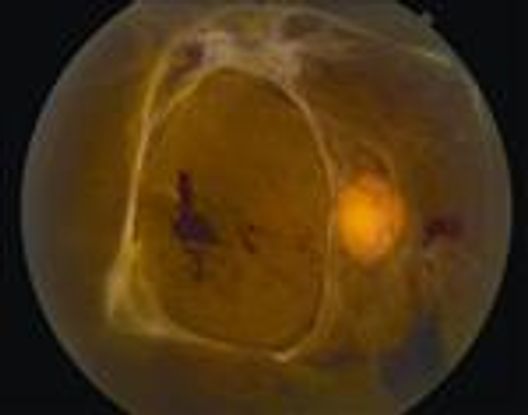
Figure 11. Tractional retinal detachment. There is associated hemorrhage due to traction on fronds of neovascular ingrowth. (© 2013 American Academy of Ophthalmology.)
Management Classification
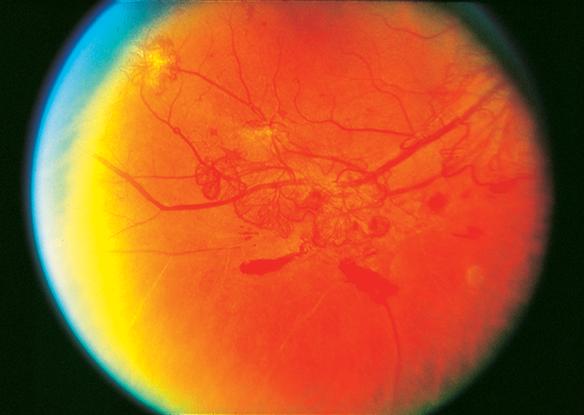
Figure 12. Moderate neovascularization elsewhere with preretinal hemorrhage. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Standard photograph 7, courtesy of ETDRS.)
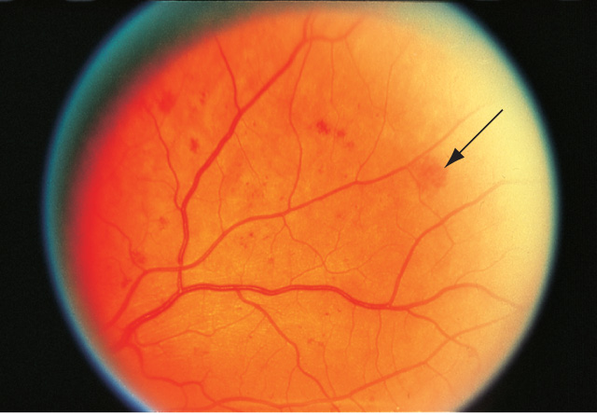
Figure 13. Diffuse intraretinal hemorrhages (arrow) and microaneurysms in nonproliferative diabetic retinopathy. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of ETDRS.)
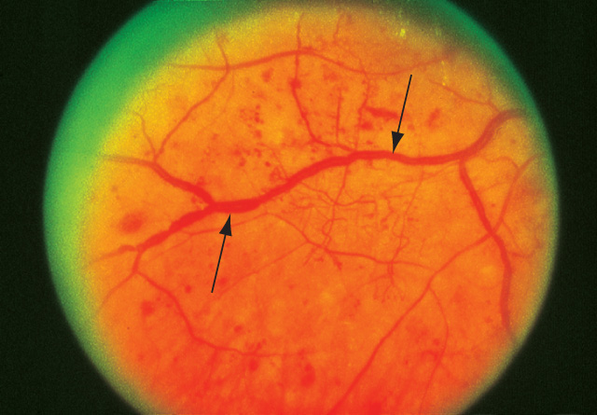
Figure 14. Venous beading in nonproliferative diabetic retinopathy. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of ETDRS.)
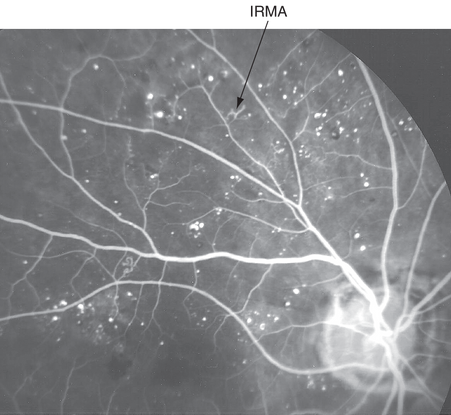
Figure 15. Intraretinal microvascular abnormalities (IRMAs) in nonproliferative diabetic retinopathy. Fluorescein angiogram showing microaneurysms, areas of nonperfusion, and intraretinal capillary remodeling. (© 2013 American Academy of Ophthalmology.)
Treatment
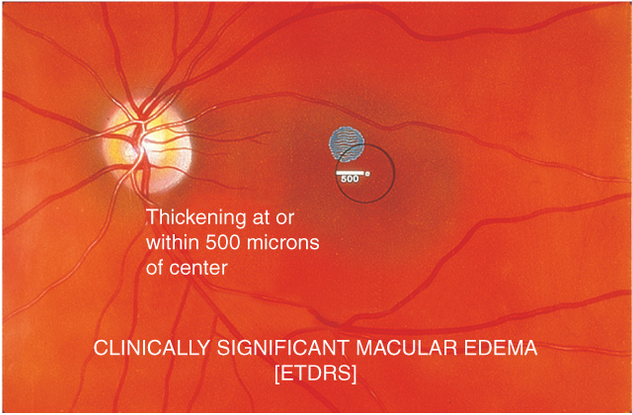
Figure 16. Clinically significant macular edema. Retinal edema located at or within 500 μm of center of macula. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of ETDRS.)
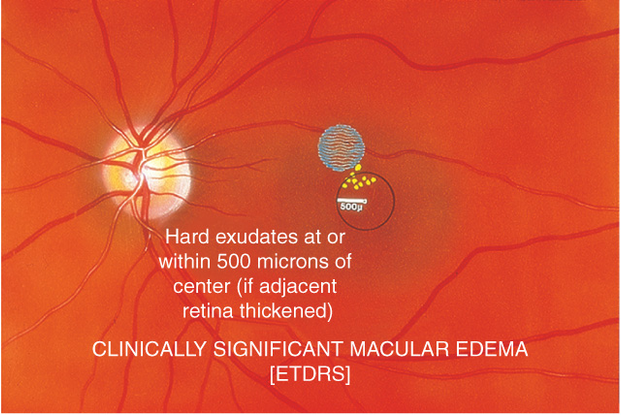
Figure 17. Clinically significant macular edema. Hard exudates ≤500 μm of center of macular if associated with adjacent edema. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of ETDRS.)
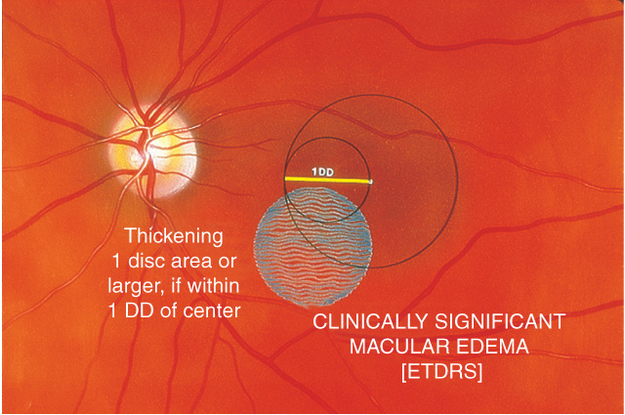
Figure 18. Clinically significant macular edema. A zone of thickening larger than 1 disc area within 1 disc diameter of the center of the macula. (Reproduced, with permission, from Schubert HD. Retina and Vitreous. Basic and Clinical Science Course, Section 12, American Academy of Ophthalmology, 2013–2014. Courtesy of ETDRS.)
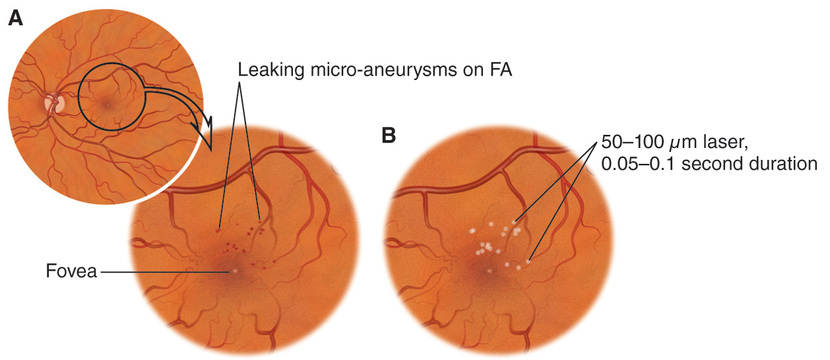
Figure 19. Treatment with focal laser photocoagulation. (Reproduced, with permission, from Dunn JP et al. Basic Techniques of Ophthalmic Surgery, American Academy of Ophthalmology, 2009.)
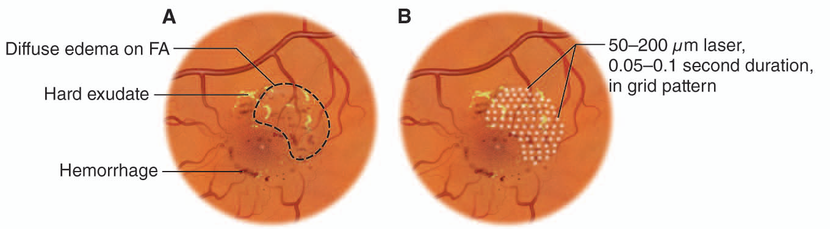
Figure 20. Treat with grid laser photocoagulation for diffuse clinically significant diabetic macular edema. (Reproduced, with permission, from Dunn JP et al. Basic Techniques of Ophthalmic Surgery, American Academy of Ophthalmology, 2009.)
Management

Figure 21. Scatter panretinal photocoagulation (© 2013 American Academy of Ophthalmology.)
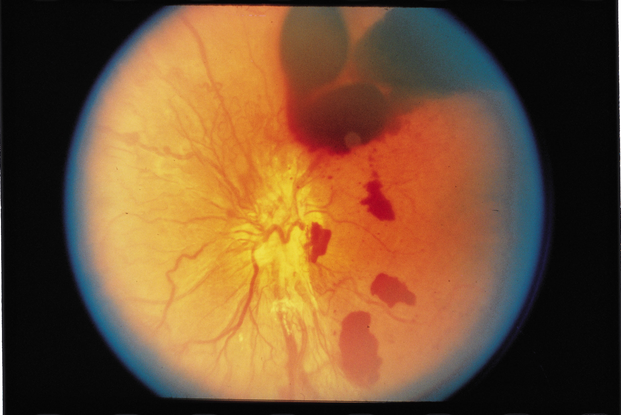
Figure 22. Vitreous hemorrhage w/decreased vision for more than 3 months. (© 2013 American Academy of Ophthalmology.)
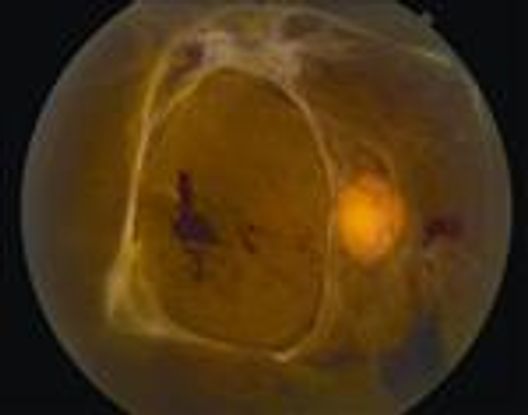
Figure 23. Traction retinal detachment involving the macula. (© 2013 American Academy of Ophthalmology.)

Figure 24. Macular epiretinal membrane or displacement of macula. (© 2013 American Academy of Ophthalmology.)
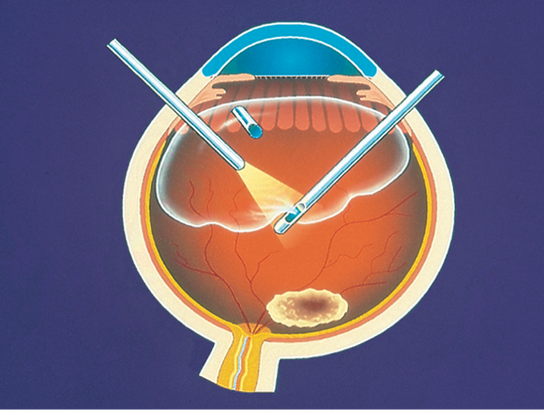
Figure 25. Pars plana vitrectomy. (© 2013 American Academy of Ophthalmology.)
Case Study
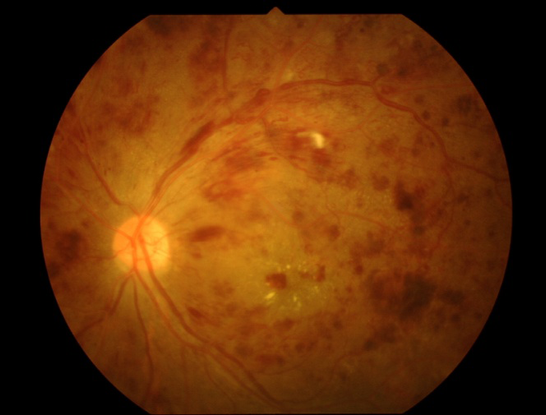
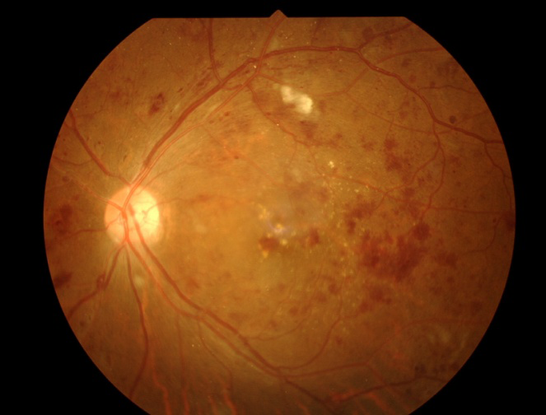
Figure 26. Proliferative diabetic retinopathy. A. Before treatment. B. One week after intravitreal injection with bevacizumab, the patient’s fundus examination showed much improvement.
REFERENCES
American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern®Guidelines. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2008 (4th printing 2012). Available at: https://www.aao.org/ppp.
Al-Adsani. Risk factors for diabetic retinopathy in Kuwaiti type 2 diabetic patients. Saudi Med J. 2007;28:579–583.
Al Alawi E, Ahmed AA. Screening for diabetic retinopathy: the first telemedicine approach in a primary care setting in Bahrain. Middle East Afr J Ophthalmol. 2012;19:295–298
al-Mahroos F, McKeigue PM. High prevalence of diabetes in Bahrainis. Associations with ethnicity and raised plasma cholesterol. Diabetes Care. 1998;21:936–942.
Al-Maskari F, El-Sadig M. Prevalence of diabetic retinopathy in the United Arab Emirates: a cross-sectional survey. BMC Ophthalmology. 2007 June 16;7:11.
Bandello F, Cunha-Vaz J, Chong NV, et al. New approaches for the treatment of diabetic macular edema: recommendations by an expert panel. Eye. 2012;26:485-493.
el Haddad OA, Saad MK. Prevalence and risk factors for diabetic retinopathy among Omani diabetics. Br J Ophthlamol.1998;82:901–906.
Heydari B, Yaghoubi G, Yaghoubi MA, Miri MR. Prevalence and risk factors for diabetic retinopathy: an Iranian eye study. Eur J Ophthalmol. 2012;22:393–397.
Janghorbani M, Amini M, Ghanbar H, Safaiee H. Incidence and risk factors for diabetic retinopathy in Isfahan, Iran. Ophthalmic Epidemiol. 2003;10:80–95.
Khan AR, Wiseberg JA, Lateef ZA, Khan SA. Prevalence and determinants of diabetic retinopathy in Al Hasa region of Saudi Arabia: primary health care centre based cross-sectional survey, 2007–2009. Middle East Afr J Ophthalmol. 2010;17:257–263.
Khandekar R. Screening and public health strategies for diabetic retinopathy in the Eastern Mediterranean region. Middle East Afr J Ophthalmol. 2012;19:178–184.
Nwosu SN. Diabetic retinopathy in Nnewi, Nigeria. Nig J Ophthamol. 2000;8:7–10.
Nwosu SN. Low vision in Nigerians with diabetes mellitus. Doc Ophthalmol. 2000;101(1):51–57.
Prokofyeva E, Zrenner E. Epidemiology of major eye diseases leading to blindness in Europe: a literature review. Ophthalmic Res. 2012;47:171–188.
Rabiu MM, Kyari F, Ezelum C, et al. Review of the publications of the Nigeria national blindness survey: methodology, prevalence, causes of blindness and visual impairment and outcome of cataract surgery. Ann Afr Med. 2012;11:125–130.
World Health Organization. “Diabetes Fact Sheet.” Geneva, Switzerland: World Health Organization, 2011.
Yau JW, Rogers SL, Kawasaki R, et al; Meta-Analysis for Eye Disease (META-EYE) Study Group. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–564.
Zhang X, Saaddine JB, Chou CF, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304:649–656.
CONTRIBUTORS
Executive Editor:
R. V. Paul Chan, MD, FACS, Weill Cornell Medical College, New York, New York
Section Editor:
Asia-Pacific:
Timothy Lai, MD
Manish Nagpal MBBS, FRCS, MS
Assistant Editors:
Swetangi D. Bhaleeya, MD, Weill Cornell Medical College; New York, New York
Kristin Chapman, MD, Weill Cornell Medical College, New York, New York
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
Michael Klufas, MD, Weill Cornell Medical College, New York, New York
Samir Patel, medical student, Weill Cornell Medical College; New York, New York
Region Contributor:
Paisan Ruamviboonsuk, MD, Department of Ophthalmology, Rajavithi Hospital, Bangkok, Thailand
Sjakon Tahija, MD, CO Klinik Mata Nusantara, Jakarta, Indonesia
Copyright © 2013 American Academy of Ophthalmology®. All Rights Reserved.