The links to each individual chapter of the Color Atlas of Gonioscopy are available at the Chapters link, below.
The best preparation for recognizing angle pathology is to become familiar with the many variations of normal. Careful gonioscopic evaluation of the anterior segment follows a routine that evaluates all visible structures in a systematic fashion. This chapter focuses on normal findings, beginning at the iris and moving to the periphery.
Iris
Examination of the iris begins centrally, looking for deposits at the pupillary border that are suggestive of pseudoexfoliation.
Moving peripherally, the contour of the iris is usually found to be flat or slightly convex. Hyperopic eyes have more convex irides, while myopic or aphakic eyes typically have flat or slightly concave irides. Abnormal convexity is noted in pupillary block, with large lenses, and with tumors and cysts of the iris and ciliary body. Abnormal concavity is seen in the pigment dispersion syndrome and the iris-retraction syndrome.
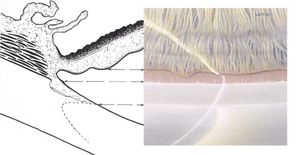
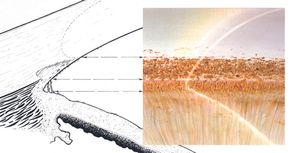
The normal iris demonstrates radial markings with crypts (5‑1, also see 1‑3). Blue irides have more prominent markings and crypts than thick, brown irides. It is valuable to compare these surface features between the two eyes. In some pathologic conditions, such as Fuchs heterochromic iridocyclitis, the normal markings are lost, giving the iris a flat, featureless appearance.
The iris also has concentric contraction rolls, which are most prominent when the pupil is large and the iris bunched. The most peripheral roll of the iris is frequently more prominent than other contraction rolls (5‑1). In some eyes this last roll can obscure visualization of the trabecular meshwork. An abnormally prominent last roll of the iris is a feature of plateau iris syndrome, a form of angle closure that is described in Chapter 8.
The iris should be examined for the presence of nevi, tumors, atrophy, iridodonesis, and abnormal pigmentation.
As the angle is approached, the stroma of the iris becomes thinner and smoother. There may be a scalloped border where the iris inserts into the face of the ciliary body.
5-1 Normal iris with distinct radial markings and crypts. As in many normal angles, the last contraction roll of the iris is prominent but does not obstruct the view of the angle structures.
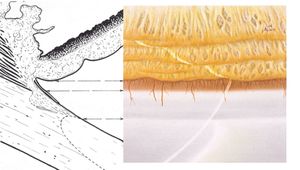
Ciliary Body Band
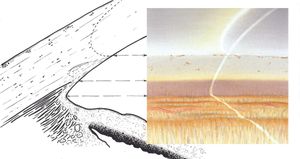
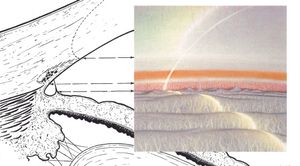
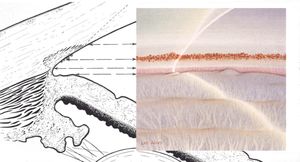
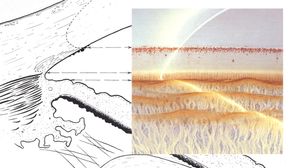
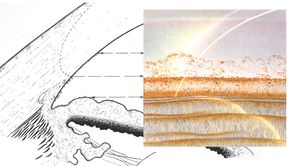
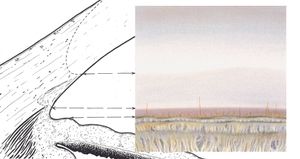
The iris usually inserts into the concave face of the ciliary body, leaving some of the ciliary body visible anterior to the iris. The ciliary body band is seen as a light gray to dark brown band located just anterior to the iris and posterior to the scleral spur (5‑2 to 5‑4).
This band can be quite wide in myopic or aphakic eyes and narrow to absent in hyperopic eyes or eyes with anterior insertions of the iris. If the ciliary body band is abnormally deep and not symmetric with the other eye, the possibility of angle recession, cyclodialysis, or unilateral high myopia must be considered. Both angle recession and cyclodialysis are described in Chapter 9.
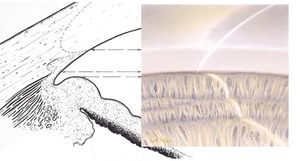
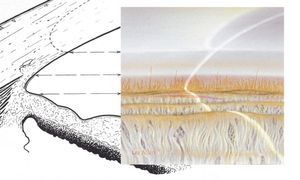
5-2 Broad, gray ciliary body band, seen most commonly in lightly pigmented eyes.
5-3 Lavender-colored ciliary body band, common with all types of iris pigmentation (superior angle).
5-4 Dark brown ciliary body band usually associated with hazel or brown irides.
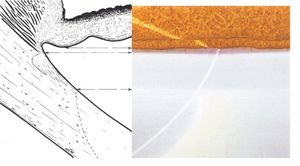
Scleral Spur
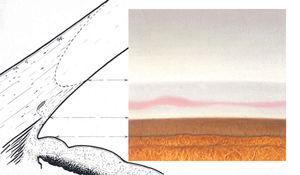
The scleral spur is a ridge of scleral tissue that lies anterior to the ciliary body band and marks the posterior border of the trabecular meshwork. It appears as a thin band that is usually white or light gray (5‑5) but which may have a yellowish cast in older individuals (5‑6). It may be difficult to distinguish from trabecular meshwork in lightly pigmented eyes except for the striking contrast of the adjacent ciliary body band (5‑7). Although the scleral spur is usually visible, it may be obscured by iris processes, a high insertion of the iris, iris bombé, peripheral anterior synechiae, or heavy pigmentation.
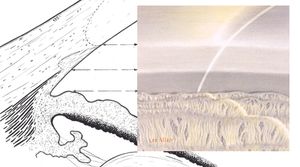
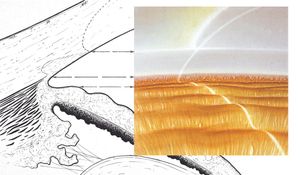
5-5 Narrow, light gray scleral spur accentuated by a low, sharp ridge at the iris root (superior angle).
5-6 Wide, yellowish scleral spur line, an appearance seen more often in the elderly. The major circle of the iris is visible.
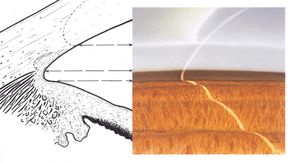
5-7 Scleral spur of the same color as the trabecular meshwork, identified only by contrast with the color of the ciliary body band.
Trabecular Meshwork
The trabecular meshwork lies between the scleral spur and Schwalbe’s line. The meshwork is nonpigmented and smooth in infants but becomes coarser and more pigmented with advancing age. Flow through the trabecular meshwork is through the posterior portion. For this reason, the posterior trabecular meshwork is generally more pigmented than the anterior trabecular meshwork. Most of the dark brown or black pigment present in the angle is intracellular, having been ingested through phagocytosis. Skin and hair color show little correlation with trabecular pigmentation (Scheie, 1957). There may be patchy areas of increased pigmentation over the circumference of the pigmented trabecular meshwork. These are located over aqueous collector channels and represent areas that have more outflow than the less pigmented areas. Patchy pigmentation is seen more frequently in eyes with glaucoma than in normal eyes (Tanchel et al, 1984).
Pigment in the angle is usually heaviest inferiorly owing to gravitational settling and aqueous circulation. With narrow angles, there can be more pigment superiorly than inferiorly as a result of apposition of the iris against trabecular meshwork (Desjardins and Parrish, 1985). Similarly, patients with pigment dispersion syndrome have been noted to be more pigmented superiorly than inferiorly during the regression phase, known as the “pigment reversal sign” (Ritch, 1996).
A nonpigmented angle is a pale gray color (5‑8). Trabecular pigmentation usually appears deep within the posterior trabecular meshwork (5‑9). Sometimes pigment is deposited on the surface of the posterior trabecular meshwork (5‑10) or over the anterior trabecular meshwork and Schwalbe’s line (5‑11). Heavy pigmentation may cover all angle structures (5‑12 and 5‑13). Increased pigmentation of the angle can be caused by many pathological processes; these are discussed in detail in Chapter 9. Heavy angle pigment can accumulate in a line anterior to Schwalbe’s line as a Sampaolesi’s line. Sampaolesi’s line is a nonspecific finding in heavily pigmented angles, whether physiologic or pathologic.The corneal wedge can help in locating Schwalbe’s line and in defining whether the pigmentation is in the trabecular meshwork or anterior to it. Systems for grading angle pigmentation are discussed in Chapter 6.
The anterior border of the trabecular meshwork is usually smooth, but it can be wavy and irregular (5‑14).
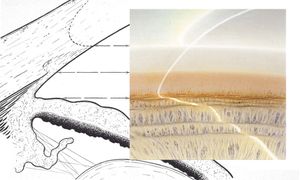
5-8 Narrow trabecular band of normal gray color (superior angle).
5-9 Deep pigment in the trabecular meshwork near Schlemm’s canal forming a smooth, brown band. A solitary iris process is present.
5-10 Discrete pigment on the surface of the trabecular meshwork overlying Schlemm’s canal.
5-11 Discrete pigment along the anterior margin of the trabecular meshwork with a few flecks anterior to Schwalbe’s line (identified by the corneal wedge).
5-12 Heavy angle pigmentation with a wavy band of pigment on the corneal endothelium anterior to Schwalbe’s line (Sampaolesi’s line).
5-13 Heavier pigment than that seen in 5‑12. The pigment obscures much of the angle anatomy and is dusted on the surface of the iris.
5-14 Irregularly wavy anterior border of the trabecular meshwork. Note the normal iris processes.
5-15 Blood in Schlemm’s canal. This can be seen in normal eyes, with increased episcleral venous pressure, in ocular hypotony, and with excessive pressure on the limbus from a large gonioscopic lens. Note that the trabecular band is wide and is darker than the adjacent cornea.
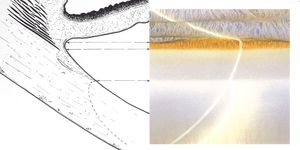
Schlemm’s Canal
In most individuals Schlemm’s canal is not visible. It lies deep within the posterior (pigmented) trabecular meshwork, anterior to the scleral spur, and becomes visible only when filled with blood (5‑15). Blood can occasionally be found in Schlemm’s canal in normal eyes. It may also be seen in situations where the flow of aqueous humor from Schlemm’s canal to the episcleral venous system is impeded. This can occur when a contact lens with a large diameter (such as a Goldmann lens) is pressed too firmly against the eye, compressing the episcleral veins. It can also be seen when the pressure in the episcleral venous system is high or when the intraocular pressure is low. Pathologic causes of blood in Schlemm’s canal are discussed in Chapter 9.
Schwalbe’s Line
Schwalbe’s line represents the anterior border of the trabecular meshwork. It is the termination of Descemet’s membrane. Schwalbe’s line is usually subtle, marked only by a slight change in color and density from trabecular meshwork to cornea (5‑16) and, occasionally, by a faint white line (5‑17). The line is often too faint to be identified, particularly in an eye with a very lightly pigmented trabecular meshwork. The corneal wedge, described in Chapter 4, is invaluable in identifying Schwalbe’s line. In most eyes the line is a flat transition zone between trabecular and corneal endothelium. In some eyes it forms a ridgelike structure (5‑18). A line that is prominent and anterior is termed “posterior embryotoxon.” This is usually a normal variant. A very prominent roll of tissue in this location is associated with the Axenfeld- Rieger syndrome (Chapter 7). Pigment deposited on and anterior to Schwalbe’s line is called a Sampaolesi’s line, as described above.
5-16 Anterior border of the trabecular meshwork marked only by a change of color and density from trabecular meshwork to the corneoscleral limbus. There are scattered iris processes (superior angle).
5-17 Multiple fine, pearly-white lines delineating the anterior border of the trabecular meshwork (superior angle).
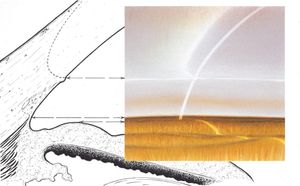
5-18 Prominent Schwalbe’s line forming a ridge. Such elevation is most frequently seen in the inferior quadrant.
Other Regions
The cornea can also be viewed gonioscopically, demonstrating pigment, keratic precipitates, or endothelial changes. The ciliary body can be examined in a widely dilated or an aniridic eye.
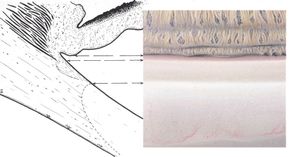
Iris Processes
Iris processes are often found in normal angles. These are uveal extensions from the iris on to the trabecular meshwork. They generally insert close to the scleral spur but sometimes insert as far anteriorly as Schwalbe’s line. Usually delicate and lacy (5‑19 and 5‑20), these processes can sometimes be so dense as to obscure the scleral spur. They are abnormally numerous and prominent in Axenfeld-Rieger syndrome (Chapter 7). Iris processes range in color from light gray (in blue-eyed individuals) to dark brown.
It is important—and occasionally difficult—to distinguish iris processes from peripheral anterior synechiae. Iris processes are usually fine wisps of iris and extend into the posterior portions of the trabecular meshwork. They usually follow the concavity of the angle recess but can bridge the angle. Iris processes do not inhibit the movement of the iris with indentation and they do not interfere with aqueous outflow. Peripheral anterior synechiae tend to be broad and irregular, attaching iris stroma to the trabecular meshwork. They bridge the angle recess, rather than follow it, and they obscure underlying structures. Synechiae inhibit posterior movement of the iris during indentation gonioscopy. They drag normal radial iris vessels with them. There is frequently pigmentation on the cornea anterior to the synechiae caused by the underlying pathology, such as inflammation or angle closure.
With traumatic angle recession, iris processes can be broken. This is a very helpful sign of recession in patients with already deep angles.
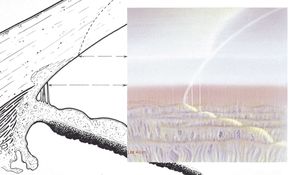
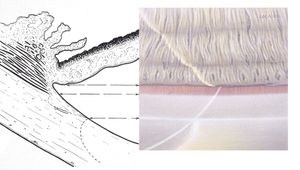
5-19 Dense band of nonpigmented iris processes bridging the angle.
5-20 Heavily pigmented iris processes against the wall of the superior angle.
Angle Blood Vessels
Typically, normal angle blood vessels have a radial orientation in the iris or form looping branches from the major arterial circle. Although the major circle is usually located in the ciliary muscle, it may occasionally be seen in the periphery of the iris. Short segments of the major circle are often visible in lightly pigmented irides and are sometimes visible in darkly pigmented irides (5‑21) (Henkind, 1964). This is in contrast to pathologic angle vessels, which tend to be fine, cross the scleral spur, and branch. They do not follow any radial or circumferential pattern. Pathologic vessels have associated fibrous tissue, which is not visible, and causes increase in intraocular pressure even before synechial closure of the angle.
Angle Width
The angle between the iris and the cornea is usually wide enough to permit a good view of all angle structures (5‑22). The angle is generally quite wide in myopic eyes (5‑23) and narrower in hyperopic eyes. Angle closure is rare in myopic eyes, although there are exceptions (van Herick et al, 1969), most notably in eyes with spherophakia. Aphakic and pseudophakic eyes tend to have rather wide angles because of the loss of lens thickness behind the iris.
Many factors determine the width of the angle, including the level of insertion of the iris into the angle, the shape of the iris, pupil size, lens thickness, and the degree of lens-iris apposition. Sometimes the iris inserts so far anteriorly that it obscures the ciliary body band, the scleral spur, and even parts of the trabecular meshwork (5‑24).
5-21 Major circle of the iris visible in the angle. This normal structure is usually seen in blue or hazel eyes.
5-22 Chamber angle of average width. In most eyes, the inferior angle is widest, the lateral quadrants are narrower, and the superior angle is narrowest.
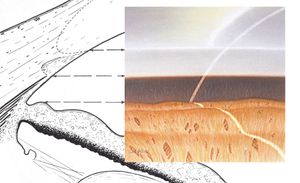
5-23 Wide chamber angle resulting from the insertion of the iris root considerably posterior to the scleral spur and from low iris rolls.
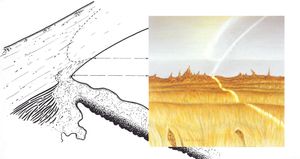
5-24 Iris root anterior to the scleral spur—an uncommon congenital variant.
The angle narrows with age. Raeder (1923 ) attributed this to increasing thickness of the lens. A study of 947 normal subjects showed that the mean age for a closed angle was 85 years, while the mean age for a Shaffer grade IV angle was 25 years (Spaeth, 1971). Van Herick et al (1969) used the slit lamp to examine 2185 individuals. They found that grade I and II angles were present in 6% of those over 60 years of age and in none of those under 20 years of age.
Usually the superior angle is the narrowest, the inferior angle is the widest, and the lateral angles are of intermediate width (Barkan et al, 1936).
Cholinergic stimulating agents, such as pilocarpine, cause the lens-iris diaphragm to move forward. This narrows the angle and makes the approach to the angle steeper. Rarely, cholinergic agents can cause pupillary block and closure of the angle. Angle narrowing caused by cholinergic agents can be reversed by anticholinergic drugs, which tend to widen the angle but can also cause crowding of the peripheral angle with dilation of the pupil. This is particularly evident in patients with plateau iris.
Uneven angle width can be caused by cysts of the iris or ciliary body, angle recession, and cyclodialysis.